What do you learn in phlebotomy class? It’s a question that often pops up for those interested in a healthcare career, especially those drawn to the hands-on nature of blood collection. Phlebotomy is more than just drawing blood; it’s a critical skill that requires precision, accuracy, and a keen understanding of anatomy, physiology, and infection control.
Phlebotomists play a vital role in healthcare, bridging the gap between patients and laboratories, ensuring that vital blood samples are collected safely and accurately for diagnosis and treatment.
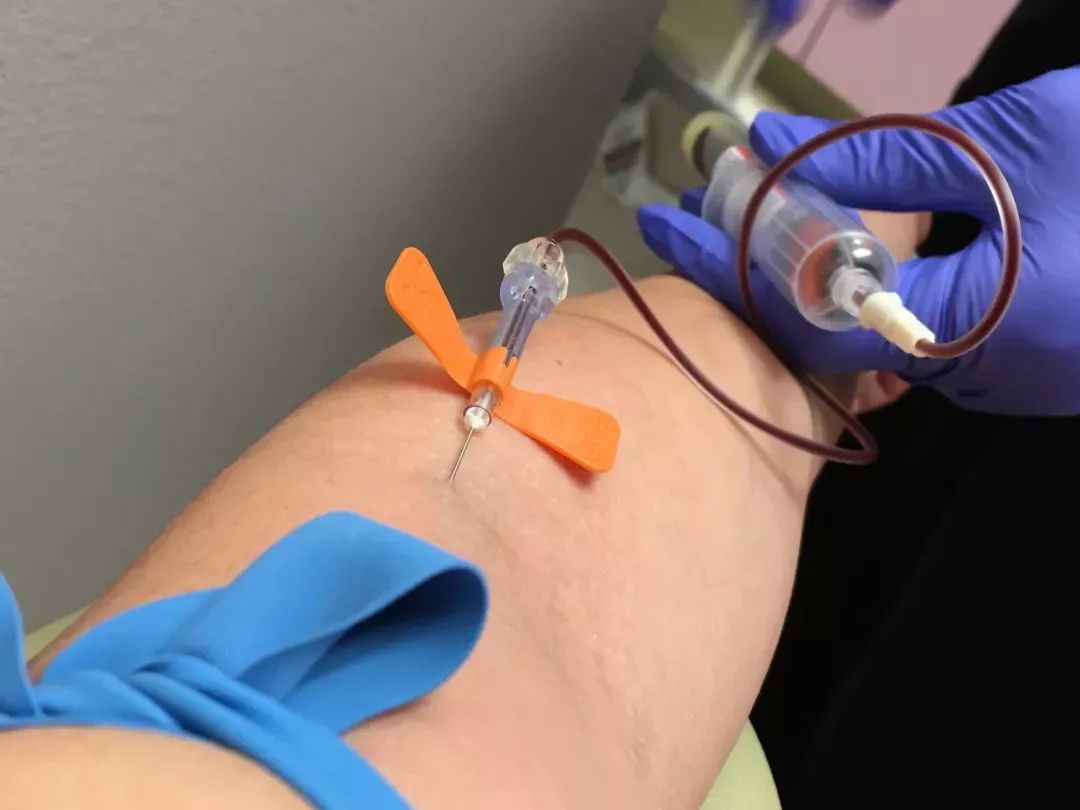
In phlebotomy class, you’ll delve into the fascinating world of blood, learning about its components, the circulatory system, and the various procedures for blood collection. You’ll master techniques like venipuncture, capillary puncture, and arterial puncture, gaining the skills to draw blood from diverse patient populations, including children and seniors.
But beyond the technical aspects, you’ll also explore the importance of patient communication, ethical considerations, and the legal and regulatory frameworks that govern the practice of phlebotomy. By the end of your training, you’ll be equipped with the knowledge and skills to become a competent and compassionate phlebotomist, ready to contribute to the healthcare system in a meaningful way.
Introduction to Phlebotomy
Phlebotomy is a vital component of healthcare, and phlebotomists play a crucial role in ensuring the smooth operation of healthcare facilities. They are the individuals responsible for collecting blood samples from patients, a task that requires precision, accuracy, and a deep understanding of safety protocols.
The Role of a Phlebotomist in Healthcare Settings
Phlebotomists are the bridge between patients and laboratory testing. They are responsible for collecting blood samples for various diagnostic and therapeutic purposes. This involves a multifaceted approach that encompasses patient interaction, blood collection techniques, and meticulous record keeping.
- Blood Collection:Phlebotomists are trained to use various techniques to collect blood samples, ensuring the accuracy and safety of the process. This includes selecting the appropriate vein, using sterile equipment, and collecting the required volume of blood. They also need to be adept at handling different types of blood collection tubes, ensuring proper labeling and storage.
- Patient Interaction:Phlebotomists interact directly with patients, explaining the procedure, answering questions, and addressing concerns. They need to be empathetic and patient, especially when dealing with anxious or apprehensive individuals. Effective communication is key to building trust and ensuring a positive patient experience.
- Record Keeping:Maintaining accurate records is crucial in phlebotomy. Phlebotomists are responsible for documenting patient information, blood collection details, and any observations or complications. These records are essential for tracking patient health, facilitating laboratory testing, and ensuring proper billing and reimbursement.
Phlebotomists are essential members of the healthcare team, working in various settings such as:
- Hospitals:Phlebotomists in hospitals are responsible for collecting blood samples for a wide range of patients, from newborns to elderly individuals, and for various purposes, including routine check-ups, emergency procedures, and specialized tests.
- Clinics:In clinics, phlebotomists often handle a smaller volume of blood collections but may specialize in specific procedures, such as drawing blood for prenatal testing or for patients with specific medical conditions.
- Laboratories:Some phlebotomists work directly in laboratories, performing blood collection procedures, processing samples, and ensuring the accuracy and quality of laboratory results.
Phlebotomists collaborate closely with other healthcare professionals, including:
- Physicians:Phlebotomists receive orders from physicians regarding the type of blood tests required, the volume of blood needed, and any special instructions for the collection process.
- Nurses:Nurses often work alongside phlebotomists, providing support and assistance, especially in challenging situations, such as drawing blood from patients with difficult veins.
- Lab Technicians:Phlebotomists work closely with lab technicians, ensuring the proper handling, processing, and analysis of blood samples. They may also be involved in the quality control procedures within the laboratory.
The Importance of Accurate and Safe Blood Collection
Accurate and safe blood collection is paramount in healthcare. Errors in blood collection can have significant consequences for patients, including:
- Misdiagnosis:Inaccurate blood test results can lead to misdiagnosis, resulting in inappropriate treatment and potentially worsening a patient’s condition.
- Treatment Errors:Misidentified blood samples or incorrect test results can lead to inappropriate medication or treatment decisions, jeopardizing patient safety.
- Patient Harm:Unsafe blood collection practices, such as using non-sterile equipment or improper venipuncture techniques, can expose patients to infection and other complications.
To ensure accurate and safe blood collection, phlebotomists adhere to strict protocols, including:
- Proper Patient Identification:Verifying patient identity using multiple identifiers is crucial to prevent misidentification and ensure the correct blood sample is collected.
- Sterile Technique:Using sterile equipment, gloves, and proper hand hygiene minimizes the risk of contamination and infection.
- Appropriate Specimen Handling:Following specific guidelines for specimen handling, including labeling, storage, and transportation, is essential to maintain the integrity of the sample and ensure accurate test results.
Ethical considerations play a significant role in phlebotomy:
- Patient Confidentiality:Phlebotomists are obligated to maintain patient confidentiality, protecting sensitive medical information and ensuring privacy during blood collection procedures.
- Informed Consent:Patients have the right to understand the procedure and its potential risks and benefits before giving consent for blood collection.
- Respect for Patient Autonomy:Phlebotomists should respect patient autonomy, allowing patients to refuse blood collection or request alternative procedures if they have concerns.
A Brief Overview of the History of Phlebotomy
Phlebotomy, the practice of drawing blood, has a long and fascinating history, dating back to ancient times.
- Ancient Times:In ancient Egypt, phlebotomy was used for therapeutic purposes, believed to balance bodily humors and treat various ailments. The practice was also common in ancient Greece and Rome, where bloodletting was considered a standard medical procedure.
- Medieval Period:During the Middle Ages, phlebotomy remained a prevalent practice, often used for a wide range of conditions, including fevers, headaches, and even mental illness. Bloodletting was often performed using leeches, which were believed to draw out “bad blood” from the body.
- Renaissance and Enlightenment:The Renaissance and Enlightenment periods saw a shift in medical thinking, with a growing emphasis on scientific observation and experimentation. While bloodletting remained common, its use became more selective, and the practice began to be questioned by some medical practitioners.
- Modern Era:The development of blood transfusions in the 19th century revolutionized the practice of phlebotomy. Blood transfusions allowed for the replacement of lost blood, significantly improving patient outcomes in cases of severe blood loss. The understanding of blood components, such as red blood cells, white blood cells, and platelets, further advanced the field of phlebotomy, leading to the development of specialized blood tests and diagnostic procedures.
Today, phlebotomy is a highly specialized and regulated field, with phlebotomists playing a crucial role in ensuring the accuracy and safety of blood collection procedures. Their dedication to patient care and their commitment to ethical practices make them vital members of the healthcare team.
Anatomy and Physiology of the Circulatory System
The circulatory system is the body’s transportation network, delivering oxygen and nutrients to cells and removing waste products. It’s a complex system made up of the heart, blood vessels, and blood. Understanding the structure and function of each component is crucial for phlebotomists, as it helps you understand the process of blood collection and its potential implications.
The Heart
The heart is a muscular organ located in the chest, slightly to the left of the center. It’s responsible for pumping blood throughout the body. The heart has four chambers: two upper chambers called atria and two lower chambers called ventricles.
- The right atrium receives deoxygenated blood from the body.
- The right ventricle pumps this deoxygenated blood to the lungs.
- The left atrium receives oxygenated blood from the lungs.
- The left ventricle pumps oxygenated blood to the rest of the body.
The heart’s rhythmic contractions, called heartbeats, are controlled by electrical impulses generated by specialized cells within the heart itself.
Blood Vessels
Blood vessels are the network of tubes that carry blood throughout the body. There are three main types of blood vessels:
- Arteries: These vessels carry oxygenated blood away from the heart. They have thick, elastic walls to withstand the high pressure of blood pumped from the heart. Arteries branch into smaller vessels called arterioles.
- Veins: These vessels carry deoxygenated blood back to the heart. They have thinner walls than arteries and contain valves to prevent backflow of blood. Veins branch into smaller vessels called venules.
- Capillaries: These are the smallest blood vessels, connecting arteries and veins. They are thin-walled, allowing for the exchange of gases, nutrients, and waste products between blood and the surrounding tissues.
Blood Components
Blood is a vital fluid that carries oxygen, nutrients, and hormones throughout the body, and removes waste products. It’s composed of plasma and various blood cells:
- Plasma: The liquid portion of blood, containing water, proteins, electrolytes, and other substances.
- Red blood cells (RBCs): These cells contain hemoglobin, a protein that binds to oxygen and carries it to the body’s tissues. They are responsible for the red color of blood.
- White blood cells (WBCs): These cells are part of the immune system, fighting infections and diseases. They are larger than RBCs and have a nucleus.
- Platelets: These are cell fragments involved in blood clotting. They stick to damaged blood vessels, forming a plug to stop bleeding.
Blood Circulation
The process of blood circulation involves the continuous flow of blood throughout the body.
The heart pumps blood through arteries to the body’s tissues. Oxygen and nutrients are exchanged in capillaries, and waste products are collected. Deoxygenated blood then flows back to the heart through veins, completing the cycle.
Equipment and Supplies
Phlebotomy involves the use of specialized equipment and supplies to ensure safe and accurate blood collection. Understanding the purpose and proper handling of these tools is essential for any phlebotomist.
Blood Collection Tubes
Blood collection tubes are the primary containers for collecting and storing blood samples. They come in various colors, each representing a different additive that helps preserve the blood for specific tests.
- Red-top tubes:Contain no additives and are used for serum testing, such as blood chemistry and serology. They allow the blood to clot naturally before the serum is separated.
- Lavender-top tubes:Contain EDTA (ethylenediaminetetraacetic acid), an anticoagulant that prevents blood clotting. These tubes are used for hematology testing, such as complete blood count (CBC).
- Light blue-top tubes:Contain sodium citrate, another anticoagulant that prevents blood clotting. These tubes are used for coagulation testing, such as prothrombin time (PT) and partial thromboplastin time (PTT).
- Green-top tubes:Contain heparin, an anticoagulant that prevents blood clotting. These tubes are used for chemistry testing, such as electrolytes and blood gases.
- Gray-top tubes:Contain sodium fluoride and potassium oxalate, which act as an anticoagulant and a glucose preservative, respectively. These tubes are used for glucose testing.
Needles
Needles are essential for drawing blood. They come in various sizes and gauges, depending on the type of blood collection and the patient’s vein size.
- Gauge:The gauge of a needle refers to its diameter. A smaller gauge number indicates a larger diameter needle, while a larger gauge number indicates a smaller diameter needle. For example, a 21-gauge needle is larger than a 23-gauge needle.
- Length:The length of a needle also varies depending on the patient’s vein depth and the type of blood collection. A shorter needle is typically used for superficial veins, while a longer needle is used for deeper veins.
Syringes
Syringes are used to draw blood from a vein. They come in various sizes, depending on the volume of blood needed for the test.
- Safety syringes:These syringes have a built-in safety mechanism that retracts the needle after use, reducing the risk of needlestick injuries.
- Disposable syringes:These syringes are used only once and then discarded. This helps to prevent the spread of infection.
Tourniquets
Tourniquets are used to constrict blood flow in a vein, making it easier to locate and draw blood. They are typically made of latex or fabric and are applied to the upper arm, just above the elbow.
- Proper application:The tourniquet should be applied snugly but not too tightly, as this can restrict blood flow and cause discomfort to the patient.
- Time limit:The tourniquet should not be left in place for more than one minute, as this can cause tissue damage.
Alcohol Swabs
Alcohol swabs are used to disinfect the skin before drawing blood. They are typically made of gauze or cotton and are soaked in isopropyl alcohol.
- Proper technique:The alcohol swab should be used in a circular motion, starting from the center of the puncture site and moving outwards. The area should be allowed to air dry completely before the needle is inserted.
- Alternatives:For patients with sensitive skin or allergies to alcohol, alternative disinfectants such as povidone-iodine swabs can be used.
Bandages
Bandages are used to cover the puncture site after blood has been drawn. They help to stop bleeding and prevent infection.
- Types of bandages:Bandages come in various sizes and materials, including adhesive bandages, gauze pads, and pressure dressings.
- Proper application:The bandage should be applied securely but not too tightly, as this can restrict blood flow.
Other Supplies
Other supplies used in phlebotomy include:
- Gloves:Gloves are worn to protect both the phlebotomist and the patient from infection.
- Sharps container:A sharps container is a puncture-resistant container used to dispose of needles and other sharp objects.
- Specimen labels:Specimen labels are used to identify blood samples and ensure they are properly labeled with the patient’s name, date of birth, and other relevant information.
- Specimen bags:Specimen bags are used to transport blood samples to the laboratory.
Proper Handling and Maintenance
- Cleanliness:All phlebotomy equipment should be kept clean and disinfected to prevent the spread of infection.
- Storage:Equipment should be stored in a cool, dry place, away from direct sunlight.
- Inspection:Equipment should be inspected regularly for damage or defects. Any damaged or defective equipment should be discarded.
5. Blood Specimen Handling and Processing
Proper handling and processing of blood specimens are crucial for obtaining accurate and reliable test results. This section will delve into the importance of proper specimen handling, different types of blood specimens and their requirements, and best practices for labeling, storing, and transporting blood specimens.
Phlebotomy class is all about mastering the art of drawing blood, which involves a lot of hands-on practice. You learn how to properly identify veins, select the right needles, and perform the blood draw with accuracy and precision. But it’s not just about the technical skills; you also learn about the importance of patient care and communication.
Think about it, if you’re drawing blood from someone, it’s important to make them feel comfortable and at ease. To understand how to effectively communicate with patients, it’s helpful to learn about the different types of learners and how to adapt your approach.
This is where the concept of tire learning active comes in. It emphasizes engaging patients in the learning process to help them better understand their condition and treatment. By understanding these concepts, phlebotomists can provide a more personalized and effective patient experience.
5.1 Importance of Proper Specimen Handling and Processing
Improper handling of blood specimens can significantly impact the accuracy of test results, potentially leading to misdiagnosis, inappropriate treatment, and adverse patient outcomes. Contamination of specimens can occur due to various factors, including improper collection techniques, inadequate storage conditions, or mishandling during transport.
- Impact on Test Results:Contamination can introduce foreign substances into the specimen, altering the composition and interfering with the analytical process. This can lead to inaccurate test results, potentially causing delays in diagnosis or treatment.
- Potential for Contamination:Common sources of contamination include bacteria, fungi, viruses, chemicals, and even particulate matter. Contamination can occur during the collection process, storage, or transportation of specimens. For instance, using a non-sterile collection tube or exposing the specimen to extreme temperatures can introduce contaminants.
- Legal and Ethical Implications:Mishandling blood specimens can have legal and ethical consequences. Providing inaccurate test results can lead to medical negligence claims and potentially jeopardize patient safety. It’s essential to adhere to strict protocols and guidelines to ensure the integrity and reliability of blood specimens.
5.2 Types of Blood Specimens and Their Requirements
Different types of blood specimens are collected for various diagnostic purposes. Each specimen type has unique characteristics, collection requirements, and storage conditions.
| Specimen Type | Description | Collection Requirements | Storage Requirements |
|---|---|---|---|
| Whole Blood | Blood collected in a tube containing an anticoagulant, which prevents clotting. |
|
|
| Serum | Blood allowed to clot, then the serum is separated from the clot. Serum contains no clotting factors. |
|
|
| Plasma | Blood collected in a tube containing an anticoagulant, then centrifuged to separate the plasma. Plasma contains clotting factors. |
|
|
5.3 Proper Techniques for Labeling, Storing, and Transporting Blood Specimens
Proper labeling, storage, and transportation of blood specimens are essential for maintaining their integrity and ensuring accurate test results.
5.3.1 Labeling
- Essential Information:Blood specimen labels must include the patient’s full name, date of birth, unique identification number (e.g., medical record number), date and time of collection, and the phlebotomist’s initials.
- Permanent, Waterproof Markers:Use permanent, waterproof markers to ensure the label is legible and resistant to fading or smudging.
- Established Protocols:Follow established protocols for labeling specimens. The specific labeling requirements may vary depending on the laboratory or healthcare facility.
5.3.2 Storing
- Controlled Temperature Environment:Maintain a controlled temperature environment for blood specimens. Different specimen types have different storage requirements.
- Storage Requirements:Whole blood and plasma specimens are typically refrigerated at 2-8°C (35.6-46.4°F), while serum specimens can be stored at room temperature or refrigerated.
- Storage Containers:Use appropriate storage containers for blood specimens. Refrigerated specimens should be stored in sealed containers to prevent contamination.
5.3.3 Transporting
- Precautions:Take necessary precautions during the transportation of blood specimens. Protect the specimens from extreme temperatures, vibration, and shocks.
- Specialized Transport Containers:Use specialized transport containers designed to maintain the integrity of blood specimens during transport. These containers often include features like temperature control, shock absorption, and leak-proof seals.
- Maintaining Integrity:Ensure the specimen’s integrity is maintained throughout transport. Avoid exposing specimens to direct sunlight or extreme temperatures.
Safety and Infection Control: What Do You Learn In Phlebotomy Class
Phlebotomy involves direct contact with patients’ blood, making it crucial to prioritize safety and infection control. Implementing strict protocols minimizes the risk of spreading infections to patients, healthcare workers, and the community.
Standard Precautions
Standard precautions are a set of infection control practices applied to all patients, regardless of their suspected or confirmed infectious status. These precautions are designed to prevent the transmission of bloodborne pathogens and other potentially infectious materials.
- Hand Hygiene: Frequent handwashing with soap and water or using alcohol-based hand rubs is essential to remove microorganisms from hands.
- Personal Protective Equipment (PPE): Gloves, gowns, masks, and eye protection should be worn when there is a risk of contact with blood or other bodily fluids.
- Safe Injection Practices: Use single-use needles and syringes and dispose of them properly in sharps containers.
- Environmental Control: Regularly clean and disinfect surfaces, equipment, and work areas to minimize the spread of germs.
Universal Precautions
Universal precautions are a subset of standard precautions that treat all patients’ blood and bodily fluids as potentially infectious. These precautions were developed in response to the HIV/AIDS epidemic and have become an integral part of infection control practices.
- Treat all patients’ blood and bodily fluids as potentially infectious.
- Wear gloves when handling blood or bodily fluids.
- Use appropriate barriers, such as gowns and masks, to prevent contact with blood or bodily fluids.
- Dispose of contaminated materials properly.
Handling Needles and Sharps
Needles and sharps are potentially hazardous materials that require careful handling and disposal.
- Never recap needles by hand.Use a one-handed scoop method or a needle recapping device.
- Dispose of needles and sharps in puncture-resistant sharps containers immediately after use.
- Never bend, break, or manipulate needles.
- Always handle sharps with caution and never leave them unattended.
Handling Other Potentially Hazardous Materials
Other potentially hazardous materials include blood specimens, laboratory samples, and contaminated equipment.
- Always wear gloves when handling blood specimens and laboratory samples.
- Transport blood specimens in leak-proof containers.
- Clean and disinfect all equipment and work areas after handling potentially hazardous materials.
- Follow proper procedures for decontamination and disposal of contaminated materials.
7. Quality Control and Accuracy in Phlebotomy
Maintaining accuracy and quality control in phlebotomy is crucial for ensuring patient safety and delivering reliable laboratory results. Errors in phlebotomy can lead to inaccurate test results, potentially delaying treatment or even causing harm to the patient. Implementing strict quality control measures throughout the entire phlebotomy process is essential to minimize errors and ensure the integrity of blood specimens.
7.1 Importance of Quality Control
Quality control is a fundamental aspect of phlebotomy, contributing to the overall efficiency and effectiveness of the process. It helps to:
- Ensure Patient Safety:By minimizing errors in patient identification, specimen labeling, and venipuncture techniques, quality control measures safeguard patients from potential harm caused by misdiagnosis or incorrect treatment.
- Maintain Reliability of Laboratory Results:Accurate blood collection and specimen handling are vital for producing reliable laboratory results. Quality control measures ensure that specimens are collected and processed correctly, minimizing the risk of contamination or degradation, which can affect test results.
- Improve Efficiency:Implementing quality control measures can streamline the phlebotomy process, reducing the need for repeat draws or specimen rejections, leading to a more efficient workflow.
7.2 Types of Quality Control Measures
Quality control measures in phlebotomy can be categorized into three main phases: pre-analytical, analytical, and post-analytical.
- Pre-analytical:This phase encompasses all activities before the actual blood collection, including:
- Patient Identification:Accurate identification of the patient is essential to ensure that the correct specimen is collected and associated with the right individual. This can involve checking patient identification bracelets, asking for verbal confirmation, and verifying the patient’s name and date of birth against the requisition form.
- Specimen Labeling:Proper labeling of blood collection tubes is crucial for tracking specimens and preventing mix-ups. Labels should include the patient’s name, date of birth, date and time of collection, and unique identification number.
- Proper Tube Selection:Choosing the appropriate blood collection tube is essential for ensuring the stability and integrity of the specimen. Different tube types contain specific additives that are necessary for various tests. For example, a tube containing an anticoagulant is required for coagulation studies, while a tube without an additive is used for serum chemistry tests.
- Venipuncture Techniques:Correct venipuncture techniques are vital for minimizing the risk of complications, such as hematomas, nerve damage, or infection. This includes proper vein selection, tourniquet application, needle size and angle of insertion, and blood flow control.
- Analytical:This phase involves the actual analysis of the blood specimen in the laboratory. Quality control measures in this phase focus on:
- Calibration and Maintenance of Laboratory Equipment:Regular calibration and maintenance of laboratory equipment, such as analyzers and microscopes, are essential for ensuring accurate and reliable test results.
- Reagent Quality:The quality of reagents used in laboratory tests is crucial for accurate results. Quality control measures include using reagents from reputable manufacturers, storing them properly, and regularly checking their expiration dates.
- Proficiency Testing:Proficiency testing involves sending samples to external laboratories for analysis to assess the accuracy and reliability of the laboratory’s own testing procedures. This helps to identify any potential biases or errors in the laboratory’s testing methods.
- Post-analytical:This phase encompasses all activities after the blood specimen is collected and analyzed in the laboratory, including:
- Specimen Transportation:Blood specimens must be transported to the laboratory in a timely and appropriate manner to maintain their integrity. This includes using appropriate containers and maintaining the proper temperature.
- Specimen Storage:Proper storage conditions are essential for preserving the stability of blood specimens until they are analyzed. This involves storing specimens at the appropriate temperature and protecting them from light or contamination.
- Specimen Analysis:Quality control measures in this phase include ensuring that specimens are analyzed according to established protocols, using the correct test methods, and interpreting results accurately.
7.3 Ensuring Accurate Blood Collection and Specimen Handling
- Venipuncture Techniques:
- Importance of Proper Vein Selection and Preparation:Selecting the appropriate vein for venipuncture is crucial for a successful and safe blood draw. Factors to consider include vein size, depth, and accessibility. The vein should be palpable and firm, with good blood flow. Before performing venipuncture, the site should be cleansed with an antiseptic solution to minimize the risk of infection.
- Positioning the Patient:
Patient Position Advantages Disadvantages Supine(Lying on their back) Easy access to veins in the antecubital fossa. May not be suitable for patients with respiratory difficulties. Sitting Comfortable for most patients. May cause vein collapse if the arm is not supported properly. Trendelenburg(Head lower than feet) Can improve vein visibility in patients with poor venous return. May be uncomfortable for some patients. - Applying Tourniquet:The tourniquet should be applied 3-4 inches above the venipuncture site. It should be tight enough to restrict venous flow but not arterial flow. The tourniquet should be left in place for no more than 1 minute to avoid hemoconcentration, which can affect test results.
- Selecting the Needle:The size of the needle used for venipuncture depends on the size and condition of the vein. Smaller needles are typically used for smaller veins, while larger needles are used for larger veins. The most commonly used needle sizes are 21 gauge and 23 gauge.
- Angle of Insertion:The needle should be inserted at a 15-30 degree angle into the vein. A shallower angle can increase the risk of missing the vein, while a steeper angle can increase the risk of puncturing through the vein.
- Blood Flow:Once the needle is inserted into the vein, blood should flow freely into the collection tube. If blood flow is slow or absent, the needle may be positioned incorrectly or the vein may be collapsed. In these cases, repositioning the needle or using a different vein may be necessary.
- Common Venipuncture Errors:Common venipuncture errors include:
- Missing the vein:This can occur if the needle is not inserted at the correct angle or if the vein is not properly palpated.
- Collapsing the vein:This can occur if the tourniquet is applied too tightly or if the needle is inserted at too steep an angle.
- Hematoma formation:This occurs when blood leaks out of the vein and into the surrounding tissues. It can be caused by improper needle insertion or excessive pressure on the venipuncture site.
- Nerve damage:This can occur if the needle punctures a nerve. It is more likely to occur if the venipuncture is performed in an area where nerves are close to the surface.
- Infection:Infection can occur if the venipuncture site is not properly cleansed or if the needle is contaminated.
- Specimen Handling:
- Importance of Proper Labeling and Identification:Proper labeling and identification of specimens are essential for ensuring that the correct specimen is associated with the correct patient and that it is analyzed appropriately. Labels should be applied to the collection tube immediately after the blood draw and should include the patient’s name, date of birth, date and time of collection, and unique identification number.
- Appropriate Storage Conditions:Different types of blood specimens require different storage conditions to maintain their integrity. For example, some specimens must be stored at room temperature, while others must be refrigerated or frozen. The specific storage conditions for each specimen type should be specified by the laboratory.
- Handling and Transportation:Blood specimens should be handled and transported carefully to prevent contamination or degradation. This includes using appropriate containers, maintaining the proper temperature, and avoiding excessive shaking or agitation.
- Documentation:Accurate documentation is essential for ensuring specimen integrity. This includes recording the date and time of collection, the type of specimen collected, the collection site, and any other relevant information.
7.4 Writing
- Procedure for Performing a Venipuncture:
- Gather Supplies:Assemble all necessary supplies, including:
- Gloves
- Tourniquet
- Antiseptic wipes
- Blood collection tubes
- Needle
- Syringe (if necessary)
- Gauze pads
- Bandage
- Label
- Requisition form
- Verify Patient Identity:Check the patient’s identification bracelet and ask for verbal confirmation of their name and date of birth. Compare this information with the requisition form.
- Explain the Procedure:Explain the venipuncture procedure to the patient and answer any questions they may have.
- Position the Patient:Have the patient sit or lie down in a comfortable position. Support their arm to prevent vein collapse.
- Select the Venipuncture Site:Palpate the antecubital fossa to locate a suitable vein. Choose a vein that is palpable, firm, and has good blood flow. Avoid veins that are too small, too deep, or close to a nerve or artery.
- Prepare the Venipuncture Site:Cleanse the venipuncture site with an antiseptic wipe, working in a circular motion from the center outwards. Allow the site to air dry completely.
- Apply the Tourniquet:Apply the tourniquet 3-4 inches above the venipuncture site. Ensure that the tourniquet is tight enough to restrict venous flow but not arterial flow. Do not leave the tourniquet in place for more than 1 minute.
- Insert the Needle:Hold the needle at a 15-30 degree angle to the skin and insert it smoothly into the vein. Observe for a flash of blood in the needle hub, indicating that the needle is properly positioned.
- Collect the Blood:Once the needle is properly positioned, attach the collection tube to the needle and allow blood to flow into the tube. Fill the tube to the appropriate level, following the manufacturer’s instructions.
- Remove the Needle:Once the collection tube is filled, remove the needle from the vein. Apply pressure to the venipuncture site with a gauze pad for at least 2 minutes to stop bleeding.
- Label the Specimen:Immediately label the collection tube with the patient’s name, date of birth, date and time of collection, and unique identification number.
- Document the Procedure:Document the venipuncture procedure in the patient’s medical record, including the date and time of collection, the type of specimen collected, the collection site, and any other relevant information.
- Dispose of Supplies:Dispose of all sharps in a designated sharps container. Dispose of other waste materials according to local regulations.
- Gather Supplies:Assemble all necessary supplies, including:
- Blood Collection Tubes:
Tube Color Additive Use Red (No additive) None Serum chemistry, serology, blood banking Lavender (EDTA) Ethylenediaminetetraacetic acid Hematology, complete blood count (CBC) Light Blue (Sodium Citrate) Sodium citrate Coagulation studies, prothrombin time (PT), partial thromboplastin time (PTT) Green (Heparin) Heparin Chemistry, STAT tests Yellow (ACD) Acid citrate dextrose DNA and HLA testing Gray (Sodium Fluoride) Sodium fluoride and potassium oxalate Glucose testing, blood alcohol levels - Checklist for Accurate Blood Collection and Specimen Handling:
- Verify patient identification.
- Select the appropriate venipuncture site.
- Cleanse the venipuncture site with an antiseptic wipe.
- Apply the tourniquet correctly.
- Select the appropriate needle size.
- Insert the needle at the correct angle.
- Collect the blood into the correct tube.
- Remove the needle and apply pressure to the venipuncture site.
- Label the specimen correctly.
- Document the procedure accurately.
- Transport the specimen to the laboratory in a timely and appropriate manner.
- Store the specimen according to the laboratory’s instructions.
8. Ethical Considerations in Phlebotomy
Ethical considerations are an integral part of phlebotomy practice, ensuring patient well-being, privacy, and rights are upheld. Phlebotomists must adhere to strict ethical guidelines to maintain professional integrity and ensure safe and ethical blood collection procedures.
8.1. Patient Confidentiality
Maintaining patient confidentiality is a crucial aspect of ethical phlebotomy practice. It is essential to protect sensitive patient information, such as medical history, test results, and personal details.
- Legal and Ethical Implications:Failure to maintain patient confidentiality can have severe legal and ethical consequences. Phlebotomists are bound by laws such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, which mandates the protection of patient health information.
Breaches of confidentiality can result in disciplinary action, fines, or even criminal charges.
- Ensuring Patient Privacy:Phlebotomists must take proactive steps to safeguard patient privacy during blood draws and handling of patient information. This includes:
- Confirming patient identity using two identifiers, such as name and date of birth, before performing any procedure.
- Performing blood draws in private areas, ensuring no unauthorized individuals are present.
- Disposing of patient information securely, shredding documents or using secure electronic systems.
- Avoiding discussions about patient information in public areas.
- Keeping patient records locked and accessible only to authorized personnel.
- Breaches of Confidentiality:Examples of breaches of patient confidentiality in phlebotomy include:
- Discussing patient information with unauthorized individuals.
- Leaving patient records unattended in public areas.
- Sharing patient information on social media platforms.
- Using patient information for personal gain.
8.2. Informed Consent
Informed consent is a fundamental ethical principle in healthcare. It ensures patients understand the procedures they are undergoing and make informed decisions about their care.
- Concept of Informed Consent:In phlebotomy, informed consent means that patients are provided with sufficient information about the blood draw procedure, including its purpose, risks, and potential benefits. They must be given the opportunity to ask questions and understand the implications of consenting or refusing the procedure.
- Essential Elements of Informed Consent:The essential elements of informed consent for a phlebotomy procedure include:
- Nature of the Procedure:Explaining the purpose and nature of the blood draw, including the type of blood test being performed.
- Risks and Benefits:Discussing the potential risks and benefits associated with the procedure, such as bruising, infection, or fainting.
- Alternatives:Informing patients about alternative methods of obtaining the necessary information, if applicable.
- Right to Refuse:Emphasizing the patient’s right to refuse the procedure without any negative consequences.
- Confidentiality:Assuring patients that their information will be kept confidential.
- Role of Phlebotomists:Phlebotomists play a crucial role in obtaining informed consent from patients. They must:
- Clearly explain the procedure in simple language.
- Answer patient questions honestly and thoroughly.
- Obtain written consent from patients, ensuring they understand the information provided.
- Document the consent process, including the date, time, and witness signature.
8.3. Ethical Dilemmas in Phlebotomy
Phlebotomists may encounter ethical dilemmas in their daily practice. It is essential to navigate these situations with empathy, professionalism, and a commitment to patient well-being.
Scenario 1: Patient Refuses a Blood Draw Due to Fear of Needles
- Ethical Considerations:The phlebotomist must respect the patient’s autonomy and right to refuse treatment. It is essential to balance the patient’s right to refuse with the potential medical benefits of the blood draw.
- Approaching the Patient:The phlebotomist should approach the patient with empathy and understanding, acknowledging their fear.
- Ask open-ended questions to understand the patient’s concerns and fears.
- Explain the procedure in detail, using clear and simple language.
- Offer reassurance and support.
- Addressing Concerns:The phlebotomist can address the patient’s concerns by:
- Demonstrating proper technique and using a smaller needle.
- Providing distractions, such as music or conversation.
- Offering a break if the patient becomes overwhelmed.
- Involving a trusted family member or friend.
- Potential Risks and Benefits:The phlebotomist should explain the potential risks and benefits of proceeding with the blood draw, weighing the patient’s medical needs against their discomfort.
- If the blood draw is essential for diagnosis or treatment, the phlebotomist should explain the potential consequences of delaying or refusing the procedure.
- If the blood draw is not critical, the phlebotomist may suggest alternative methods of obtaining the necessary information.
Scenario 2: Patient Requests a Blood Draw Without a Doctor’s Order
- Ethical Considerations:The phlebotomist must prioritize patient safety and well-being. Performing a blood draw without a doctor’s order can potentially expose the patient to unnecessary risks or lead to misdiagnosis.
- Potential Risks and Benefits:The phlebotomist should carefully consider the potential risks and benefits of fulfilling the patient’s request.
- Risks:The blood draw may be unnecessary or inappropriate, potentially leading to misdiagnosis or unnecessary treatment.
- Benefits:The patient may be seeking information about their health or may have a specific reason for wanting the blood draw.
- Legal and Ethical Obligations:The phlebotomist’s legal and ethical obligations require them to obtain a doctor’s order before performing a blood draw. They should:
- Educate the patient about the importance of a doctor’s order.
- Explain the potential risks and benefits of proceeding without a doctor’s order.
- Encourage the patient to consult with their doctor.
- If the patient insists on proceeding without a doctor’s order, the phlebotomist should document the situation and inform their supervisor.
- Ensuring Patient Safety:The phlebotomist must ensure the patient’s safety and well-being, regardless of the circumstances. This includes:
- Thoroughly reviewing the patient’s medical history and any relevant information.
- Performing a thorough assessment of the patient’s condition.
- Taking appropriate precautions to minimize the risk of complications.
- Monitoring the patient closely during and after the blood draw.
Scenario 3: Phlebotomist Observes a Colleague Mishandling Patient Blood Samples
- Ethical Considerations:The phlebotomist has a responsibility to report any unsafe or unethical practices that could compromise patient safety or confidentiality. Failure to report such incidents could have serious consequences for the patients involved.
- Potential Consequences of Not Reporting:Not reporting the incident could lead to:
- Compromised patient safety due to improper handling of blood samples.
- Inaccurate test results, leading to misdiagnosis or inappropriate treatment.
- Breaches of patient confidentiality.
- Legal and ethical liability for the phlebotomist.
- Legal and Ethical Obligations:The phlebotomist has a legal and ethical obligation to report any unsafe or unethical practices. They should:
- Document the incident, including the date, time, and details of the observed behavior.
- Report the incident to their supervisor or a designated authority.
- Follow the facility’s policies and procedures for reporting unsafe or unethical practices.
- Ensuring Safety and Confidentiality:The phlebotomist must ensure the safety and confidentiality of patient information while reporting the incident. They should:
- Avoid discussing the incident with unauthorized individuals.
- Protect the identity of the colleague involved.
- Focus on the behavior observed, not personal opinions or judgments.
- Follow the facility’s policies for handling confidential information.
9. Common Blood Tests and Their Significance

Blood tests are a common and important part of medical care. They can help diagnose a wide range of conditions, monitor your health, and track the effectiveness of treatment. This section will explain some of the most common blood tests, what they measure, and what the results can tell you about your health.
Comprehensive Metabolic Panel (CMP), What do you learn in phlebotomy class
A Comprehensive Metabolic Panel (CMP) is a blood test that measures a group of substances in your blood. These substances provide information about your body’s metabolism, which is the process of how your body uses food for energy and growth.
- Glucose:This is your blood sugar level. High glucose levels can indicate diabetes, while low levels can indicate hypoglycemia.
- Electrolytes:These are minerals that carry an electric charge. Electrolytes help control your body’s fluid balance, nerve function, and muscle function. Abnormal electrolyte levels can indicate dehydration, kidney problems, or other conditions.
- Liver Enzymes:These enzymes are released into your blood when your liver is damaged. Elevated liver enzymes can indicate liver disease, hepatitis, or other conditions.
- Kidney Function Tests:These tests measure how well your kidneys are filtering waste products from your blood. Abnormal kidney function tests can indicate kidney disease or damage.
- Protein:Protein levels in your blood can indicate problems with your liver, kidneys, or other organs.
- Calcium:Calcium is important for strong bones, healthy teeth, and nerve function. Abnormal calcium levels can indicate bone disease, kidney problems, or other conditions.
Complete Blood Count (CBC)
A Complete Blood Count (CBC) measures the different types of blood cells in your blood. These cells include red blood cells, white blood cells, and platelets.
- Red Blood Cells:These cells carry oxygen throughout your body. A low red blood cell count can indicate anemia, while a high count can indicate polycythemia vera.
- White Blood Cells:These cells fight infection. A high white blood cell count can indicate infection or inflammation, while a low count can indicate a weakened immune system.
- Platelets:These cells help stop bleeding. A low platelet count can indicate a bleeding disorder, while a high count can indicate certain types of cancer.
Thyroid Stimulating Hormone (TSH) Test
The Thyroid Stimulating Hormone (TSH) test measures the level of TSH in your blood. TSH is a hormone produced by the pituitary gland in your brain. It stimulates the thyroid gland to produce thyroid hormones, which regulate your metabolism.
- High TSH levels:High TSH levels can indicate hypothyroidism, a condition where your thyroid gland doesn’t produce enough thyroid hormone.
- Low TSH levels:Low TSH levels can indicate hyperthyroidism, a condition where your thyroid gland produces too much thyroid hormone.
Lipid Panel
A Lipid Panel measures the levels of different types of fats (lipids) in your blood. These fats include cholesterol and triglycerides.
- Cholesterol:Cholesterol is a type of fat that is essential for cell function. However, high cholesterol levels can increase your risk of heart disease.
- Triglycerides:Triglycerides are another type of fat that is stored in your body for energy. High triglyceride levels can also increase your risk of heart disease.
Liver Function Tests (LFTs)
Liver Function Tests (LFTs) measure the levels of certain enzymes and proteins in your blood. These substances are produced by your liver and can indicate liver damage or disease.
- AST and ALT:These are enzymes that are released into your blood when your liver is damaged. Elevated levels of AST and ALT can indicate liver disease, hepatitis, or other conditions.
- ALP:This is an enzyme that is found in your liver, bones, and intestines. Elevated levels of ALP can indicate liver disease, bone disease, or other conditions.
- Bilirubin:Bilirubin is a yellow pigment that is produced when your body breaks down red blood cells. High levels of bilirubin can indicate liver disease, gallstones, or other conditions.
Kidney Function Tests
Kidney Function Tests measure the levels of certain substances in your blood, such as creatinine and urea nitrogen. These substances are waste products that are normally filtered out of your blood by your kidneys.
- Creatinine:Creatinine is a waste product that is produced by your muscles. High levels of creatinine can indicate kidney damage or disease.
- Urea Nitrogen:Urea nitrogen is another waste product that is produced by your body. High levels of urea nitrogen can also indicate kidney damage or disease.
HbA1c Test
The HbA1c test measures the amount of glucose attached to red blood cells. This test provides an average picture of your blood sugar levels over the past 2-3 months.
- High HbA1c levels:High HbA1c levels can indicate diabetes or poor blood sugar control.
- Low HbA1c levels:Low HbA1c levels can indicate that your blood sugar is well controlled.
Electrolyte Panel
An Electrolyte Panel measures the levels of certain minerals in your blood. These minerals, called electrolytes, carry an electric charge and help control your body’s fluid balance, nerve function, and muscle function.
- Sodium:Sodium helps regulate your body’s fluid balance. Abnormal sodium levels can indicate dehydration, kidney problems, or other conditions.
- Potassium:Potassium is important for nerve and muscle function. Abnormal potassium levels can indicate kidney problems, heart problems, or other conditions.
- Chloride:Chloride helps regulate your body’s fluid balance. Abnormal chloride levels can indicate dehydration, kidney problems, or other conditions.
- Calcium:Calcium is important for strong bones, healthy teeth, and nerve function. Abnormal calcium levels can indicate bone disease, kidney problems, or other conditions.
- Magnesium:Magnesium is important for nerve and muscle function. Abnormal magnesium levels can indicate kidney problems, heart problems, or other conditions.
- Phosphate:Phosphate is important for bone health and energy production. Abnormal phosphate levels can indicate kidney problems, bone disease, or other conditions.
Prostate-Specific Antigen (PSA) Test
The Prostate-Specific Antigen (PSA) test measures the level of PSA in your blood. PSA is a protein produced by the prostate gland.
- Elevated PSA levels:Elevated PSA levels can indicate prostate cancer, but they can also be caused by other conditions, such as benign prostatic hyperplasia (BPH) or prostatitis.
C-Reactive Protein (CRP) Test
The C-Reactive Protein (CRP) test measures the level of CRP in your blood. CRP is a protein that is produced by your liver in response to inflammation.
- Elevated CRP levels:Elevated CRP levels can indicate infection, inflammation, or other conditions.
Special Considerations for Pediatric and Geriatric Patients
Phlebotomy procedures require special considerations when working with pediatric and geriatric patients. These populations often present unique challenges due to their developmental stages, physical limitations, and varying medical conditions. It is crucial for phlebotomists to adapt their techniques and approach to ensure safe, accurate, and comfortable blood collection experiences for these patients.
Pediatric Patients
Pediatric patients require a gentle and understanding approach. Their smaller veins and delicate skin necessitate specific techniques and equipment.
Techniques and Modifications
- Smaller Needles and Tubes:Using smaller needles and tubes reduces discomfort and minimizes the risk of bruising or hematoma formation.
- Butterfly Needles:Butterfly needles are often preferred for pediatric patients, as they offer greater flexibility and control during venipuncture.
- Warm Compresses:Applying a warm compress to the venipuncture site can help dilate veins and make them easier to locate.
- Distraction Techniques:Engaging children in conversation, singing songs, or allowing them to play with toys can help distract them from the procedure.
- Parental Involvement:Encouraging parents or guardians to be present during the procedure can provide comfort and reassurance to the child.
Challenges and Solutions
- Vein Visibility:Finding veins in children can be challenging due to their smaller size and sometimes deeper location. Using a vein finder device can assist in locating suitable veins.
- Movement and Anxiety:Children may be anxious or restless during the procedure. Using a restraint system or having a parent hold the child can help minimize movement.
- Pain Management:Applying a topical anesthetic cream to the venipuncture site can help reduce pain and discomfort.
Geriatric Patients
Geriatric patients often have fragile veins, thinner skin, and may experience conditions like osteoporosis or arthritis, making venipuncture more challenging.
Techniques and Modifications
- Gentle Approach:Using a gentle touch and avoiding excessive pressure during venipuncture is crucial to minimize discomfort and potential bruising.
- Smaller Needles and Tubes:As with pediatric patients, using smaller needles and tubes is recommended to reduce the risk of complications.
- Warm Compresses:Warm compresses can be helpful for dilating veins in older adults, making them easier to access.
- Proper Positioning:Ensuring the patient is comfortable and properly positioned can help facilitate a successful venipuncture.
- Clear Communication:Communicating clearly and patiently with older adults is essential to ensure they understand the procedure and feel at ease.
Challenges and Solutions
- Fragile Veins:Older adults often have fragile veins that are more susceptible to collapse. Using a smaller needle and applying gentle pressure can help prevent this.
- Thinner Skin:Thinning skin in older adults can make venipuncture more difficult and increase the risk of bruising. Applying a tourniquet for a shorter period and using a smaller needle can minimize these risks.
- Multiple Medical Conditions:Older adults often have multiple medical conditions that may affect their ability to tolerate venipuncture. It is important to be aware of any medications or conditions that may impact the procedure.
Legal and Regulatory Requirements
As a phlebotomist, you’re not just drawing blood; you’re working within a complex legal and regulatory framework. Understanding these requirements is essential for safe, ethical, and compliant practice.
Regulatory Bodies and Professional Organizations
Several organizations play a crucial role in setting standards and ensuring quality in phlebotomy. These include:
- The Clinical Laboratory Improvement Amendments (CLIA): This federal law regulates all laboratory testing, including phlebotomy. CLIA sets standards for personnel qualifications, quality control, and proficiency testing.
- The Occupational Safety and Health Administration (OSHA): OSHA focuses on workplace safety and health, including regulations related to bloodborne pathogens and sharps safety.
- The Centers for Disease Control and Prevention (CDC): The CDC provides guidance on infection control and prevention, including recommendations for handling blood and bodily fluids.
- The American Society for Clinical Pathology (ASCP): This professional organization offers certification for phlebotomists and provides continuing education resources.
These organizations issue guidelines, regulations, and standards that phlebotomists must adhere to in their daily practice.
Common Legal and Regulatory Issues in Phlebotomy
Here are some common legal and regulatory issues phlebotomists encounter:
- Patient Consent: Obtaining informed consent from patients before drawing blood is essential. This means explaining the procedure, potential risks, and benefits in a way the patient understands. Failure to obtain consent can lead to legal action.
- Confidentiality: Phlebotomists handle sensitive patient information, including medical records and test results. Maintaining confidentiality is critical, and breaches can result in serious consequences.
- Privacy: Protecting patient privacy is essential. This involves ensuring that patient information is only accessed by authorized personnel and that appropriate measures are taken to safeguard their privacy.
- Negligence: If a phlebotomist’s actions cause harm to a patient, they may be held liable for negligence. This could involve improper technique, failure to follow safety protocols, or mishandling of blood specimens.
- Compliance with Regulations: Phlebotomists must stay informed about changes in regulations and guidelines issued by relevant organizations. Failure to comply can lead to fines, sanctions, or even loss of licensure.
12. Career Opportunities and Professional Development
Phlebotomy is a rewarding career with diverse opportunities for growth. From entry-level positions to specialized roles, there are many paths you can take to advance your career in this field. This section will explore the various career paths available to phlebotomists, the importance of continuing education and professional development, and resources that can help you advance your career.
Career Paths
Phlebotomy offers a range of career paths, from entry-level positions to specialized roles. These paths provide opportunities for professional growth and advancement, allowing you to tailor your career to your interests and goals.
- Entry-Level Positions:Entry-level positions in phlebotomy provide a solid foundation for a career in the field. These roles typically involve performing basic phlebotomy procedures and handling blood specimens.
- Advanced Roles:With experience and further education, phlebotomists can advance to more specialized and challenging roles, such as laboratory assistant, medical technologist, or phlebotomy supervisor.
- Specialized Areas:Phlebotomy skills can be applied to various specialized areas, such as forensic phlebotomy, research phlebotomy, and pediatric phlebotomy.
| Career Path | Typical Job Responsibilities | Required Education and Certifications | Average Salary Expectations | Potential Growth Opportunities |
|---|---|---|---|---|
| Phlebotomy Technician | Drawing blood from patients, labeling and processing specimens, maintaining equipment, adhering to safety protocols | High school diploma or equivalent, phlebotomy certification | $30,000
| Advance to laboratory assistant, blood bank technician, or specialized phlebotomy roles |
| Specimen Processor | Receiving, sorting, and processing blood specimens, preparing samples for testing, maintaining laboratory records | High school diploma or equivalent, phlebotomy certification | $28,000
| Advance to laboratory technician, quality control specialist, or supervisor roles |
| Blood Bank Technician | Collecting and processing blood donations, performing blood typing and crossmatching, maintaining blood bank inventory | Associate’s degree in medical technology or related field, phlebotomy certification | $35,000
| Advance to blood bank supervisor, research technician, or transfusion medicine specialist |
| Laboratory Assistant | Assisting medical technologists with laboratory procedures, performing basic laboratory tests, maintaining laboratory equipment | Associate’s degree in medical technology or related field, phlebotomy certification | $38,000
| Advance to medical technologist, laboratory supervisor, or research assistant |
| Medical Technologist | Performing a wide range of laboratory tests, analyzing and interpreting test results, reporting findings to physicians | Bachelor’s degree in medical technology or related field, certification by ASCP or equivalent | $50,000
| Advance to laboratory supervisor, research scientist, or faculty position |
| Phlebotomy Supervisor | Supervising phlebotomy staff, scheduling appointments, training new employees, ensuring quality control and compliance with regulations | Bachelor’s degree in healthcare administration or related field, phlebotomy certification, experience in phlebotomy | $45,000
| Advance to laboratory manager, regional supervisor, or director of phlebotomy services |
| Forensic Phlebotomy | Collecting and processing blood specimens for legal investigations, ensuring chain of custody, adhering to forensic protocols | Associate’s degree in criminal justice or related field, phlebotomy certification, forensic training | $40,000
| Advance to forensic laboratory technician, crime scene investigator, or forensic scientist |
| Research Phlebotomy | Collecting and processing blood specimens for research studies, adhering to research protocols, ensuring data integrity | Bachelor’s degree in biology, chemistry, or related field, phlebotomy certification, research experience | $42,000
| Advance to research technician, research coordinator, or research scientist |
| Pediatric Phlebotomy | Drawing blood from children, using specialized techniques and calming strategies, providing comfort and support to patients | High school diploma or equivalent, phlebotomy certification, pediatric training | $32,000
| Advance to pediatric laboratory technician, pediatric phlebotomy supervisor, or pediatric research technician |
Continuing Education and Professional Development
Continuing education is essential for phlebotomists to stay up-to-date with the latest advancements in the field, maintain their certifications, and enhance their skills.
- Maintaining Certification Requirements:Many phlebotomy certifications require continuing education credits for renewal. These credits can be earned through various courses, workshops, and conferences.
- Staying Up-to-Date on New Technologies and Procedures:The field of phlebotomy is constantly evolving with the introduction of new technologies and procedures. Continuing education helps phlebotomists stay abreast of these changes and enhance their skills.
- Expanding Knowledge and Skills:Continuing education courses and programs can help phlebotomists expand their knowledge and skills in specialized areas, such as pediatric phlebotomy, forensic phlebotomy, or advanced phlebotomy techniques.
- Improving Patient Care:Continuing education can help phlebotomists improve their communication skills, patient interaction techniques, and understanding of patient needs, leading to better patient care.
- Phlebotomy Proficiency Courses:These courses provide hands-on training and review of phlebotomy techniques, best practices, and safety protocols.
- Advanced Phlebotomy Techniques Workshops:These workshops focus on specialized phlebotomy techniques, such as drawing blood from difficult veins or performing arterial punctures.
- Bloodborne Pathogens Training:This training is mandatory for healthcare workers and provides information on the risks of bloodborne pathogens, prevention strategies, and proper handling of infectious materials.
- Safety and Quality Assurance Seminars:These seminars cover topics related to laboratory safety, quality control, and compliance with regulatory requirements.
Resources for Career Advancement
There are various resources available to phlebotomists to help them advance their careers, including professional organizations, online learning platforms, industry publications, and networking events.
- Professional Organizations:Professional organizations provide networking opportunities, continuing education resources, and advocacy for phlebotomists.
- Online Learning Platforms:Online learning platforms offer a wide range of phlebotomy courses and programs, providing flexibility and convenience for continuing education.
- Industry Publications and Journals:Industry publications and journals keep phlebotomists informed about the latest trends, research, and advancements in the field.
- Networking Events and Conferences:Networking events and conferences provide opportunities to connect with other phlebotomists, learn about new technologies and procedures, and explore career opportunities.
- American Society for Clinical Pathology (ASCP):The ASCP is a professional organization for laboratory professionals, including phlebotomists. It offers certification programs, continuing education courses, and networking opportunities.
- National Phlebotomy Association (NPA):The NPA is a professional organization dedicated to promoting the advancement of phlebotomy. It offers certification programs, continuing education resources, and advocacy for phlebotomists.
- Coursera, edX, Khan Academy:These online learning platforms offer a wide range of courses and programs in healthcare, including phlebotomy. They provide flexible and affordable options for continuing education.
- Clinical Laboratory News, Phlebotomy Today:These industry publications provide news, articles, and research related to laboratory medicine, including phlebotomy. They keep phlebotomists informed about the latest trends and advancements in the field.
- ASCP Annual Meeting, NPA National Conference:These annual conferences provide opportunities for phlebotomists to network with colleagues, attend educational sessions, and explore career opportunities.
Phlebotomy in Research and Clinical Trials

Phlebotomy plays a crucial role in research and clinical trials, providing valuable insights into human health and disease. It is essential for collecting blood samples that are used for a wide range of scientific investigations and clinical evaluations.
Blood Sample Collection in Research Settings
Phlebotomists in research settings are responsible for collecting blood samples from participants in a way that ensures accuracy, safety, and adherence to strict protocols. This involves understanding the specific requirements of each research study and following standardized procedures for sample collection and handling.
Specific Requirements and Procedures
- Informed Consent:Participants in research studies must provide informed consent before any blood sample collection. This means they must understand the purpose of the study, the risks and benefits involved, and their right to withdraw from the study at any time.
- Study Protocols:Research studies have detailed protocols outlining the specific types of blood samples required, the timing of collection, and the handling procedures. Phlebotomists must strictly adhere to these protocols to ensure data integrity and consistency.
- Sample Labeling and Tracking:Blood samples collected for research purposes must be accurately labeled with the participant’s unique identifier, the date and time of collection, and any other relevant information. This ensures proper tracking and identification of samples throughout the study.
- Sample Processing and Storage:Blood samples are often processed and stored according to specific research requirements. This may involve separating the blood components, such as plasma or serum, or storing the samples at specific temperatures to maintain their integrity.
Examples of Research Studies Involving Phlebotomy
Phlebotomy is integral to numerous research studies across various fields, including:
Clinical Trials
Phlebotomy is crucial in clinical trials to monitor the efficacy and safety of new drugs or treatments. Blood samples are collected at different time points to assess changes in blood parameters, such as:
- Blood cell counts:To assess the effects of a treatment on red blood cell production or white blood cell function.
- Blood chemistry:To monitor changes in liver function, kidney function, or other organ systems.
- Drug levels:To ensure that the drug is being absorbed and metabolized appropriately.
Epidemiology Studies
Phlebotomy is used in epidemiological studies to investigate the prevalence of diseases and risk factors in populations. Blood samples can be analyzed for biomarkers, such as:
- Genetic markers:To identify individuals at risk for specific diseases.
- Infectious agents:To determine the prevalence of infectious diseases in a population.
- Environmental toxins:To assess exposure to environmental toxins and their impact on health.
Pharmacokinetic Studies
Pharmacokinetic studies use phlebotomy to investigate how the body absorbs, distributes, metabolizes, and eliminates drugs. Blood samples are collected at different time points after drug administration to measure:
- Drug concentration:To determine the rate of drug absorption and elimination.
- Drug metabolites:To understand how the body breaks down the drug.
Advanced Phlebotomy Techniques
/drawing-blood-157428091-596418db3df78cdc68c06347.jpg)
Advanced phlebotomy techniques, such as arterial puncture and central line access, require specialized knowledge and skills. These procedures are typically performed by experienced phlebotomists or other healthcare professionals, and they involve a higher level of risk than standard venipuncture. This section will provide a comprehensive guide to these techniques, including anatomy, procedure, complications, and clinical applications.
Arterial Puncture
Arterial puncture is a procedure used to obtain arterial blood samples for various diagnostic tests, such as blood gas analysis, arterial blood pressure monitoring, and arterial blood cultures. Arterial blood differs from venous blood in its oxygen content, which is higher in arterial blood.
- The radial artery is located on the thumb side of the wrist, just below the base of the thumb. It is relatively superficial and easy to palpate. The brachial artery is located in the upper arm, just inside the elbow.
It is larger than the radial artery and has a stronger pulse. The femoral artery is located in the groin, just below the inguinal ligament. It is the largest artery in the lower extremities and has a deep, strong pulse.
- Patient preparation for an arterial puncture involves positioning the patient comfortably, typically with the arm extended and supported. The puncture site should be cleaned with an antiseptic solution, and the patient should be informed of the procedure and potential risks.
- The puncture technique involves selecting a suitable needle, typically a 22-gauge or 23-gauge needle. The needle should be inserted at a 45-degree angle into the artery, with the bevel facing upwards. Pressure should be applied to the artery both proximal and distal to the puncture site to prevent bleeding.
- Post-procedure care involves applying pressure to the puncture site for several minutes to ensure hemostasis. The puncture site should be monitored for bleeding or hematoma formation. The patient should be instructed to avoid strenuous activity and to report any unusual symptoms to their healthcare provider.
- Potential complications associated with arterial puncture include hematoma, arterial spasm, and nerve damage. Hematoma can occur if the needle punctures a vein or if pressure is not applied adequately. Arterial spasm can occur if the artery is irritated by the needle or if the patient is anxious.
Nerve damage can occur if the needle punctures a nerve or if the nerve is compressed during the procedure.
Central Line Access
Central venous catheters are long, thin tubes inserted into a large vein, typically in the neck, chest, or groin. They provide access to the central venous system, which allows for the administration of medications, fluids, and blood products.
- Peripherally inserted central catheters (PICCs) are inserted into a vein in the arm and threaded into a large vein in the chest. PICCs are typically used for long-term medication administration and are less invasive than other types of central venous catheters.
- Tunneled central venous catheters are inserted into a vein in the chest or neck and tunneled under the skin to a subcutaneous pocket. Tunneled catheters are typically used for long-term medication administration and are less prone to infection than PICCs.
- Implanted ports are small, flat devices that are surgically implanted under the skin. A port is connected to a central venous catheter that is inserted into a large vein in the chest. Implanted ports are typically used for long-term medication administration and are very discreet.
- Flushing a central venous catheter involves injecting a small amount of saline solution or heparin solution into the catheter to prevent occlusion.
- Dressing changes for central venous catheters involve removing the old dressing, cleaning the insertion site, and applying a new dressing.
- Troubleshooting common problems associated with central venous catheters involves identifying the cause of the problem and taking appropriate steps to resolve it. For example, if a central venous catheter is occluded, it may need to be flushed or replaced.
If a central venous catheter is infected, it may need to be removed and replaced.
The Future of Phlebotomy
The field of phlebotomy is constantly evolving, driven by technological advancements and changing healthcare needs. These developments are shaping the role of phlebotomists, creating new opportunities and challenges. This section will explore some of the emerging trends and technologies in phlebotomy and their potential impact on the profession.
Emerging Trends and Technologies in Phlebotomy
The future of phlebotomy is intertwined with advancements in technology and healthcare practices. Some key trends shaping the field include:
- Point-of-Care Testing (POCT):This involves performing laboratory tests at or near the patient’s bedside, eliminating the need for sample transportation and reducing turnaround times. POCT devices are becoming increasingly sophisticated, enabling phlebotomists to perform a wider range of tests, such as blood glucose monitoring, blood gas analysis, and even some basic chemistry tests.
- Automation and Robotics:Automation is playing a growing role in phlebotomy, particularly in high-volume laboratories. Robotic systems can automate tasks such as sample handling, labeling, and analysis, freeing up phlebotomists to focus on patient interaction and more complex procedures.
- Artificial Intelligence (AI) and Machine Learning:AI and machine learning algorithms are being used to analyze large datasets of patient information, including laboratory results. These technologies can help identify patterns and trends, leading to more accurate diagnoses and personalized treatment plans. Phlebotomists may play a crucial role in collecting and managing data that fuels these AI systems.
- Telehealth and Remote Monitoring:The rise of telehealth is enabling patients to receive healthcare services remotely. This trend is also impacting phlebotomy, with the development of home-based blood collection kits and remote patient monitoring systems. Phlebotomists may be involved in training patients on how to use these technologies and providing support remotely.
Questions Often Asked
What is the job outlook for phlebotomists?
The job outlook for phlebotomists is positive, with projected growth in the healthcare field. Demand for skilled phlebotomists is expected to remain strong, offering ample career opportunities.
How long does it take to become a phlebotomist?
The length of training varies, but you can typically become a certified phlebotomist within a few months to a year, depending on the program you choose.
What are the typical salaries for phlebotomists?
Salaries vary based on experience, location, and employer, but phlebotomists generally earn a competitive wage.
What are some common misconceptions about phlebotomy?
Many people think that phlebotomy is just about drawing blood, but it involves much more, including patient interaction, safety protocols, and understanding the importance of accurate blood collection.