A student learns what information about acute pancreatitis? This painful condition affects the pancreas, a vital organ responsible for digestion and blood sugar regulation. Understanding the causes, symptoms, and treatment of acute pancreatitis is crucial for anyone seeking to learn more about this serious health issue.
Acute pancreatitis is a sudden inflammation of the pancreas, an organ located in the abdomen. It can be a serious condition, but with prompt diagnosis and treatment, most people recover fully. In this guide, we’ll explore the causes, symptoms, diagnosis, treatment, and prevention of acute pancreatitis.
We’ll also delve into the potential complications and discuss how to manage the condition and live a healthy life after an episode.
What is Acute Pancreatitis?
Acute pancreatitis is a painful inflammation of the pancreas, a vital organ in the digestive system. It can be a serious condition, but with prompt treatment, most people recover fully.
The Role of the Pancreas in Digestion
The pancreas plays a crucial role in digestion by producing enzymes that help break down food and hormones that regulate blood sugar levels. The pancreas secretes digestive enzymes, such as lipase, amylase, and protease, into the small intestine through a duct called the pancreatic duct.
These enzymes break down fats, carbohydrates, and proteins, respectively. The pancreas also produces hormones like insulin and glucagon, which regulate blood sugar levels.
Key Characteristics of Acute Pancreatitis
Acute pancreatitis is characterized by sudden onset of severe abdominal pain, often radiating to the back. Other common symptoms include nausea, vomiting, fever, and increased heart rate. The inflammation in acute pancreatitis can cause the pancreas to become swollen and tender.
In severe cases, the inflammation can damage the pancreas, leading to complications such as:
- Pancreatic necrosis:This occurs when the pancreatic tissue dies. It is a serious complication that can lead to infection and organ failure.
- Fluid accumulation in the abdomen (ascites):This can occur due to leakage of pancreatic fluid into the abdomen.
- Pseudocyst formation:These are fluid-filled sacs that can form in the pancreas or surrounding tissues.
- Organ failure:In severe cases, acute pancreatitis can lead to organ failure, such as respiratory failure, kidney failure, or liver failure.
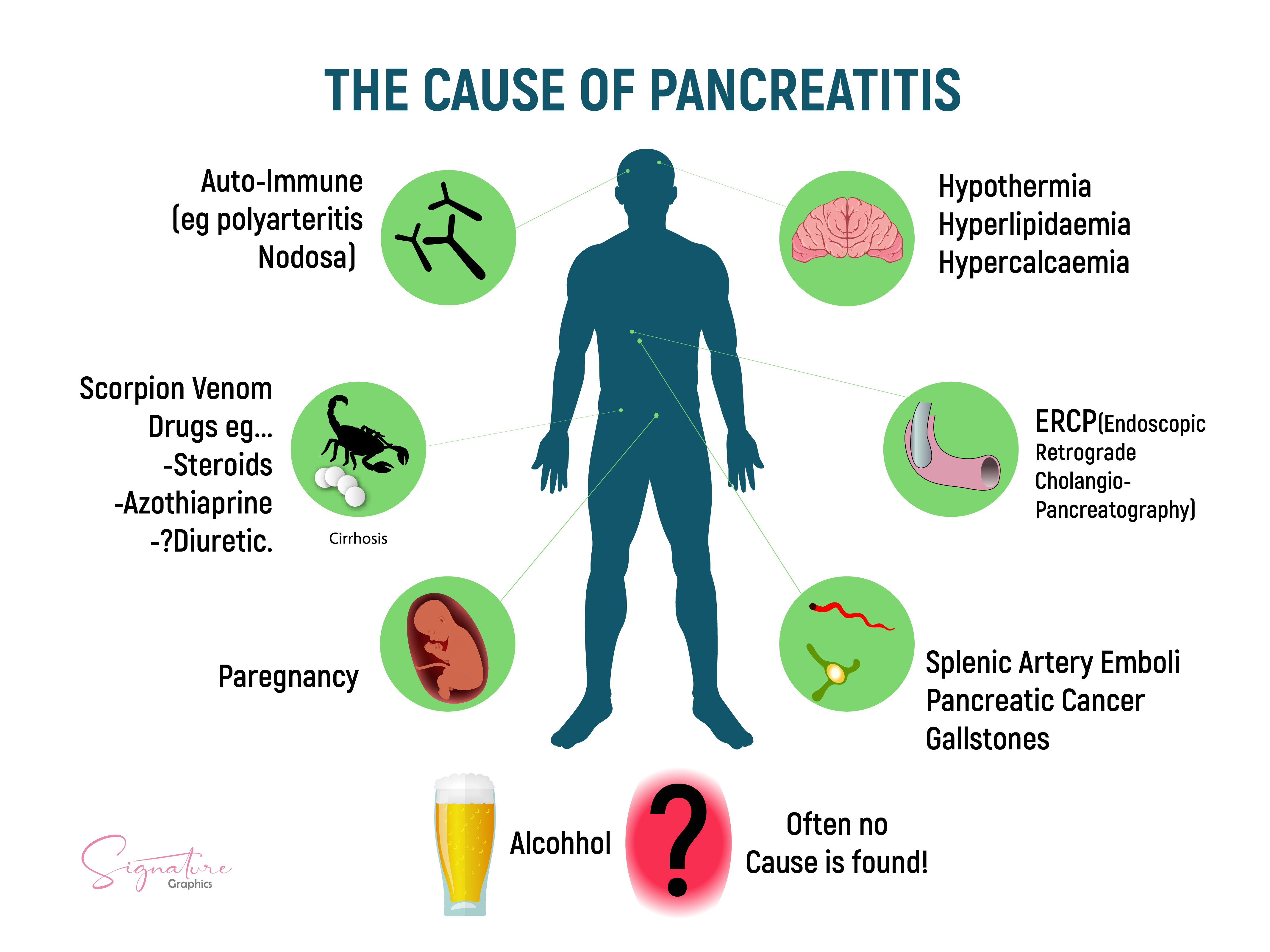
Causes of Acute Pancreatitis
Acute pancreatitis is a serious condition that involves inflammation of the pancreas, a gland located in the upper abdomen. This inflammation can cause severe pain, digestive problems, and even life-threatening complications. While the exact cause of acute pancreatitis can be difficult to pinpoint, certain factors are known to significantly increase the risk of developing this condition.
Common Causes
The most common causes of acute pancreatitis are alcohol abuse and gallstones. Understanding these triggers is crucial for prevention and effective management of the condition.
- Alcohol Abuse: Excessive alcohol consumption is a major contributor to acute pancreatitis. Alcohol directly damages pancreatic cells, leading to inflammation and impaired function. This damage can be exacerbated by the presence of certain alcohol-related toxins, such as acetaldehyde. Individuals who consume large quantities of alcohol, especially hard liquor, are at a higher risk of developing pancreatitis.
Chronic alcohol abuse can lead to recurrent pancreatitis, which can ultimately progress to chronic pancreatitis, a more severe and irreversible form of the disease.
- Gallstones: Gallstones are small, hard deposits that form in the gallbladder. When these stones become lodged in the bile duct, which connects the gallbladder to the pancreas, they can block the flow of pancreatic enzymes. This blockage leads to a buildup of pressure within the pancreas, causing inflammation and damage.
Gallstone-associated pancreatitis is a common cause of acute pancreatitis, accounting for a significant proportion of cases.
- High Triglycerides: Elevated levels of triglycerides, a type of fat found in the blood, can also contribute to acute pancreatitis. High triglycerides can form tiny fat globules that can block the pancreatic duct, leading to inflammation. This is particularly common in individuals with severe hypertriglyceridemia, a condition characterized by extremely high levels of triglycerides.
- Certain Medications: Some medications, such as steroids, antibiotics, and anticonvulsants, can increase the risk of acute pancreatitis. These drugs can cause direct damage to pancreatic cells or interfere with the normal flow of pancreatic enzymes. While the risk of pancreatitis associated with medication is relatively low, it is important to be aware of this potential side effect, especially in individuals with other risk factors.
- Infections: Viral or bacterial infections can also trigger acute pancreatitis. These infections can directly affect the pancreas or cause systemic inflammation that spreads to the organ. Common viral causes include mumps virus and cytomegalovirus, while bacterial infections can be caused by organisms like E.
coli and Salmonella.
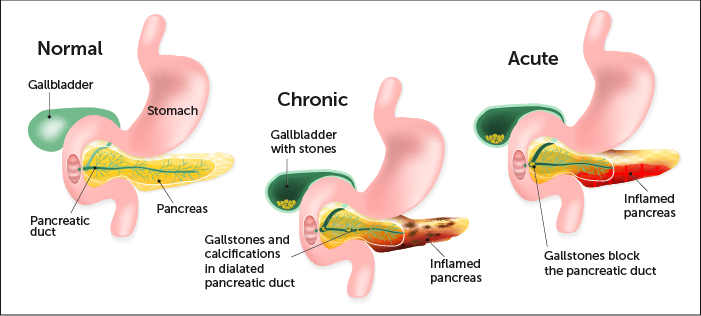
Gallstones and Pancreatitis
Gallstones are a common cause of acute pancreatitis, accounting for a significant proportion of cases. Gallstones can block the pancreatic duct, leading to a buildup of pressure within the pancreas, causing inflammation and damage. The prevalence of gallstone-associated pancreatitis is estimated to be around 40-50% of all cases.
Other Causes
While alcohol abuse and gallstones are the most common causes, other less frequent factors can also contribute to acute pancreatitis. These include:
- Medications: Certain medications, such as steroids, antibiotics, and anticonvulsants, can increase the risk of acute pancreatitis. These drugs can cause direct damage to pancreatic cells or interfere with the normal flow of pancreatic enzymes. While the risk of pancreatitis associated with medication is relatively low, it is important to be aware of this potential side effect, especially in individuals with other risk factors.
- Infections: Viral or bacterial infections can also trigger acute pancreatitis. These infections can directly affect the pancreas or cause systemic inflammation that spreads to the organ. Common viral causes include mumps virus and cytomegalovirus, while bacterial infections can be caused by organisms like E.
coli and Salmonella.
- Trauma: Blunt abdominal trauma, such as a car accident or a fall, can cause direct injury to the pancreas, leading to inflammation. Penetrating injuries, such as stab wounds or gunshot wounds, can also damage the pancreas and trigger pancreatitis. Trauma-induced pancreatitis is relatively rare but can be very serious, as it often involves significant tissue damage.
Writing
Acute pancreatitis, an inflammation of the pancreas, is a serious condition with diverse causes. The most common culprits are alcohol abuse and gallstones. Alcohol consumption, particularly excessive and chronic, directly damages pancreatic cells, leading to inflammation and impaired function. Gallstones, when lodged in the bile duct, obstruct the flow of pancreatic enzymes, causing pressure buildup and inflammation.
Other contributing factors include high triglyceride levels, certain medications, and infections. Medications like steroids, antibiotics, and anticonvulsants can cause pancreatic cell damage or interfere with enzyme flow. Viral infections, such as mumps and cytomegalovirus, and bacterial infections from organisms like E.
coli and Salmonella can directly affect the pancreas or trigger systemic inflammation. Finally, trauma, both blunt and penetrating, can cause direct injury to the pancreas, leading to pancreatitis. Understanding these causes is crucial for prevention and effective management of acute pancreatitis.
Table
| Cause | Mechanism | Prevalence ||—|—|—|| Alcohol abuse | Direct toxic effects on pancreatic cells | 30-40% || Gallstones | Obstruction of the pancreatic duct | 40-50% || Medications | Drug-induced toxicity | 5-10% || Infections | Viral or bacterial inflammation | 5-10% || Trauma | Direct injury to the pancreas | 1-5% |
3. Symptoms of Acute Pancreatitis
Acute pancreatitis, a painful inflammation of the pancreas, can manifest with a range of symptoms that vary in severity and frequency. Understanding these symptoms is crucial for early diagnosis and prompt medical intervention, as timely treatment can significantly improve outcomes.
The Five Most Common Symptoms of Acute Pancreatitis
The most common symptom of acute pancreatitis is severe abdominal pain. This pain is often described as a sharp, stabbing sensation that can radiate to the back. It typically occurs in the upper abdomen, just below the ribs. Other common symptoms include nausea, vomiting, fever, and abdominal distension.
- Abdominal pain:This is the most common symptom, experienced by almost all patients with acute pancreatitis (95-100%).
- Nausea and vomiting:These symptoms are also very common, occurring in 80-90% of patients.
- Fever:A fever is present in about 70% of patients with acute pancreatitis.
- Abdominal distension:This symptom, characterized by a swollen abdomen, is observed in approximately 60% of patients.
- Tenderness:Abdominal tenderness, which is pain upon palpation, is present in about 50% of patients.
The Intensity and Duration of Pain
The pain associated with acute pancreatitis is often described as excruciating and can last for several days. It typically worsens after eating, especially fatty foods, and may radiate to the back. The pain can be so severe that it makes it difficult for patients to lie down or find a comfortable position.
The intensity of the pain can fluctuate, but it usually reaches its peak within the first 24-48 hours.
Nausea and Vomiting
Nausea and vomiting are common symptoms of acute pancreatitis, often occurring together. They can be triggered by the inflammation and irritation of the pancreas, as well as the release of digestive enzymes into the bloodstream. These symptoms can contribute to dehydration, making it important for patients to stay hydrated.
Fever
Fever is a common symptom of acute pancreatitis, indicating the body’s inflammatory response. The temperature typically ranges from 100.4°F (38°C) to 102.2°F (39°C). A fever can be caused by infection, inflammation, or complications of pancreatitis, such as a pancreatic abscess.
Abdominal Distension and Tenderness
Abdominal distension and tenderness are common symptoms of acute pancreatitis, resulting from inflammation and fluid accumulation in the abdomen. The distension can be caused by fluid buildup in the peritoneal cavity, a condition known as ascites. Tenderness occurs when the inflamed pancreas or surrounding tissues are pressed upon.
Key Symptoms of Acute Pancreatitis
Acute pancreatitis is a serious condition that requires prompt medical attention. The most common symptoms include severe abdominal pain, nausea, vomiting, fever, and abdominal distension. If you experience these symptoms, it’s important to seek immediate medical care.
Diagnosis of Acute Pancreatitis

Diagnosing acute pancreatitis involves a combination of medical history, physical examination, laboratory tests, and imaging studies. The doctor will carefully evaluate your symptoms, medical history, and risk factors to determine the best course of action.
Physical Examination
The physical examination plays a crucial role in diagnosing acute pancreatitis. The doctor will assess your overall health, including your vital signs such as blood pressure, heart rate, and temperature. They will also check for signs of abdominal pain, tenderness, and distention.
Blood Tests
Blood tests are essential for diagnosing acute pancreatitis and assessing its severity. The doctor will order several tests, including:
- Amylase and Lipase Levels:These enzymes are produced by the pancreas, and their levels rise significantly in acute pancreatitis. Elevated levels of amylase and lipase in the blood strongly suggest pancreatitis.
- Complete Blood Count (CBC):This test helps determine the presence of inflammation and infection. Elevated white blood cell count may indicate infection or inflammation.
- Liver Function Tests (LFTs):These tests assess the function of the liver, which can be affected by pancreatitis.
- Blood Glucose Levels:Pancreatitis can affect the pancreas’ ability to regulate blood sugar, so checking blood glucose levels is important.
Imaging Techniques
Imaging techniques provide visual information about the pancreas and surrounding organs. Common imaging tests include:
- Ultrasound:Ultrasound uses sound waves to create images of the pancreas. It can help identify inflammation, swelling, and fluid collections in the pancreas.
- Computed Tomography (CT) Scan:A CT scan uses X-rays to create detailed images of the pancreas and surrounding structures. It can detect inflammation, swelling, and fluid collections, and it can also identify complications like pseudocysts.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP is a specialized procedure that combines endoscopy and X-ray imaging to visualize the bile ducts and pancreatic duct. It is typically performed if gallstones or other problems in the biliary system are suspected as the cause of pancreatitis. ERCP can also be used to remove gallstones or to place stents to improve drainage from the pancreas.
Treatment of Acute Pancreatitis
Treating acute pancreatitis focuses on managing symptoms, preventing complications, and allowing the pancreas to heal. This involves supportive care, pain management, and addressing any underlying infections. In severe cases, surgical interventions may be necessary.
Supportive Care
Supportive care is crucial in managing acute pancreatitis. It involves providing the body with the necessary resources to recover. This includes:
- Fluid Replacement:Intravenous (IV) fluids are administered to prevent dehydration, which can worsen the condition. This helps maintain blood pressure and organ function.
- Nutritional Support:Patients may require temporary cessation of oral intake to allow the pancreas to rest. In some cases, nutritional support is provided through IV fluids or nasogastric tubes until the pancreas heals.
- Pain Management:Pain is a common symptom of acute pancreatitis. Medications like IV opioids are used to control pain and improve comfort.
Pain Medications
Pain relief is a priority in acute pancreatitis. While IV opioids are commonly used, other medications may also be administered, depending on the severity of the pain. These may include:
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs):NSAIDs can help reduce inflammation and pain, but their use may be limited in some cases due to potential complications.
- Antispasmodics:These medications help relax the muscles in the digestive system, reducing spasms that can contribute to pain.
Antibiotics
Antibiotics are used to treat infections that may develop in acute pancreatitis. Infections can occur due to complications like pancreatic necrosis (tissue death) or abscess formation. Antibiotics are prescribed based on the specific type of infection and the patient’s overall condition.
Surgical Interventions
Surgical interventions may be necessary in severe cases of acute pancreatitis. These procedures aim to address complications like:
- Pancreatic Necrosis:Removal of necrotic (dead) pancreatic tissue to prevent infection and sepsis.
- Abscesses:Drainage of abscesses (collections of pus) to relieve pressure and promote healing.
- Bile Duct Obstruction:Procedures to relieve blockage in the bile duct, which can be a cause of pancreatitis.
6. Complications of Acute Pancreatitis
Acute pancreatitis, while often resolving on its own, can sometimes lead to serious complications that can significantly impact a patient’s health. Understanding these complications is crucial for timely diagnosis and appropriate management.
Pancreatic Necrosis and Infection
Pancreatic necrosis, the death of pancreatic tissue, is a serious complication of acute pancreatitis. It occurs when the pancreas becomes inflamed and damaged, leading to tissue death. This necrosis can become infected, leading to a life-threatening condition called infected pancreatic necrosis.
The development of pancreatic necrosis is often associated with severe acute pancreatitis and can be influenced by factors such as:* Severity of pancreatitis:More severe cases of pancreatitis are more likely to develop necrosis.
Age
Older individuals tend to have a higher risk of developing necrosis.
Underlying conditions
Certain medical conditions, such as diabetes and alcoholism, can increase the risk.
Delayed diagnosis and treatment
Prompt diagnosis and treatment can help prevent the development of necrosis.Infected pancreatic necrosis can be life-threatening and often requires aggressive treatment, including antibiotics and surgical intervention.
Ascites
Ascites is the accumulation of fluid in the abdominal cavity. In the context of acute pancreatitis, ascites can develop due to:* Increased capillary permeability:The inflammation in the pancreas can cause leakage of fluid from blood vessels into the abdominal cavity.
Decreased lymphatic drainage
The inflammation can also disrupt the lymphatic system, which normally removes excess fluid from the abdomen.
Increased pressure in the portal vein
The portal vein, which carries blood from the digestive system to the liver, can become blocked due to inflammation, leading to increased pressure and fluid leakage.Ascites can cause abdominal distention, discomfort, and difficulty breathing. Treatment often involves draining the fluid and addressing the underlying cause.
Organ Failure
Acute pancreatitis can lead to organ failure in multiple organs, including:* Respiratory failure:Inflammation can cause fluid buildup in the lungs, leading to difficulty breathing.
Renal failure
The kidneys can be damaged by inflammation and decreased blood flow, leading to impaired kidney function.
Cardiac failure
Pancreatitis can affect the heart, leading to decreased pumping function.
Hepatic failure
The liver can be affected by inflammation and decreased blood flow, leading to impaired liver function.Organ failure is a serious complication that can be life-threatening and requires intensive care.
Chronic Pancreatitis
Acute pancreatitis can sometimes progress to chronic pancreatitis, a condition characterized by persistent inflammation and damage to the pancreas. This can lead to:* Persistent pain:Chronic pancreatitis can cause persistent abdominal pain, even in the absence of an acute attack.
Malabsorption
The pancreas plays a vital role in digestion, and damage to the pancreas can lead to malabsorption of nutrients.
Diabetes
Chronic pancreatitis can damage the cells in the pancreas that produce insulin, leading to diabetes.Risk factors for developing chronic pancreatitis after an episode of acute pancreatitis include:* Alcohol abuse:Alcoholism is a major risk factor for both acute and chronic pancreatitis.
Genetic predisposition
Some individuals may be genetically predisposed to developing pancreatitis.
A student learning about acute pancreatitis will likely encounter information about its causes, symptoms, and treatment. It’s a lot to take in, just like learning a new craft, like crocheting. If you’re curious about how long it takes to learn to crochet, you can check out this resource: how long does it take to learn how to crochet.
Just like mastering crocheting, understanding acute pancreatitis requires dedication and a willingness to learn.
Recurring episodes of acute pancreatitis
Repeated episodes of acute pancreatitis can increase the risk of developing chronic pancreatitis.Management of chronic pancreatitis often involves:* Pain management:Pain medications can help alleviate the pain associated with chronic pancreatitis.
Dietary modifications
A low-fat diet can help reduce digestive problems.
Enzyme replacement therapy
Pancreatic enzyme supplements can help improve digestion.
Insulin therapy
Insulin therapy may be required if diabetes develops.
Common Complications of Acute Pancreatitis
| Complication | Potential Causes | Symptoms | Treatment |
|---|---|---|---|
| Pancreatic Necrosis | Severe pancreatitis, age, underlying conditions, delayed diagnosis | Severe abdominal pain, fever, elevated white blood cell count | Antibiotics, surgical intervention |
| Ascites | Increased capillary permeability, decreased lymphatic drainage, increased portal vein pressure | Abdominal distention, discomfort, difficulty breathing | Fluid drainage, addressing underlying cause |
| Organ Failure | Inflammation, decreased blood flow | Respiratory distress, impaired kidney function, heart failure, liver dysfunction | Intensive care, supportive measures |
| Chronic Pancreatitis | Alcohol abuse, genetic predisposition, recurring acute pancreatitis | Persistent abdominal pain, malabsorption, diabetes | Pain management, dietary modifications, enzyme replacement therapy, insulin therapy |
Prevention of Acute Pancreatitis
Preventing acute pancreatitis is crucial as it can significantly reduce the risk of developing this painful and potentially life-threatening condition. While some causes are beyond our control, adopting healthy habits and addressing underlying health issues can significantly lower your chances of experiencing this condition.
Reducing Alcohol Consumption, A student learns what information about acute pancreatitis
Excessive alcohol intake is a leading cause of acute pancreatitis. Reducing or eliminating alcohol consumption is a critical step in preventing this condition.
- Moderate Drinking: For individuals who choose to consume alcohol, moderation is key. The recommended daily limit for women is one drink and for men, two drinks.
- Alcohol-Free Days: Incorporating alcohol-free days into your weekly routine can help reduce your overall alcohol intake and minimize the risk of pancreatitis.
- Long-Term Abstinence: If you have a history of pancreatitis or are at high risk, abstaining from alcohol altogether is strongly recommended.
Managing Gallstones
Gallstones, small, hard deposits that form in the gallbladder, are another common cause of acute pancreatitis. Managing gallstones effectively can significantly reduce your risk.
- Regular Checkups: Regular medical checkups, especially if you have a family history of gallstones, can help detect gallstones early. Early detection allows for prompt treatment, reducing the risk of complications like pancreatitis.
- Healthy Diet: Maintaining a healthy diet, rich in fruits, vegetables, and whole grains, can help prevent the formation of gallstones. Avoid high-fat foods and processed foods that can contribute to their formation.
- Weight Management: Obesity is a significant risk factor for gallstones. Maintaining a healthy weight through regular exercise and a balanced diet can help reduce your risk.
- Surgical Intervention: If gallstones are present and causing symptoms, surgical removal of the gallbladder (cholecystectomy) may be recommended. This procedure effectively eliminates the risk of pancreatitis caused by gallstones.
Healthy Lifestyle Choices
Adopting healthy lifestyle choices can play a significant role in preventing acute pancreatitis.
- Balanced Diet: A balanced diet rich in fruits, vegetables, and whole grains can contribute to overall health and reduce the risk of pancreatitis. Limit high-fat foods, processed foods, and sugary drinks.
- Regular Exercise: Regular physical activity can help maintain a healthy weight, reduce inflammation, and improve overall health, lowering the risk of pancreatitis.
- Smoking Cessation: Smoking is a significant risk factor for pancreatitis. Quitting smoking can significantly reduce your risk of developing this condition.
Early Diagnosis and Treatment of Underlying Conditions
Certain underlying medical conditions, such as high triglycerides, hyperparathyroidism, and certain genetic disorders, can increase the risk of pancreatitis. Early diagnosis and treatment of these conditions are crucial in preventing pancreatitis.
- Regular Medical Checkups: Regular medical checkups can help identify and manage underlying conditions that could contribute to pancreatitis. This proactive approach can significantly reduce your risk.
- Following Treatment Plans: If you have been diagnosed with a condition that increases your risk of pancreatitis, strictly following your treatment plan is crucial. This includes taking prescribed medications and making necessary lifestyle changes.
Prognosis of Acute Pancreatitis
The prognosis of acute pancreatitis, meaning the expected outcome, depends on several factors, including the severity of the attack, the underlying cause, and the patient’s overall health. Early diagnosis and prompt treatment are crucial for improving the chances of a successful recovery.
Factors Influencing Prognosis
The severity of the pancreatitis is a major determinant of the prognosis. Mild cases usually resolve within a week with supportive care, while severe cases can lead to life-threatening complications. Other factors that can affect the prognosis include:
- Underlying cause:Pancreatitis caused by alcohol abuse or gallstones tends to have a poorer prognosis than pancreatitis caused by other factors.
- Age:Older adults are at higher risk for complications and mortality.
- Presence of other medical conditions:Patients with underlying conditions such as diabetes, heart disease, or kidney disease may have a more challenging recovery.
- Nutritional status:Malnutrition can worsen the severity of pancreatitis and increase the risk of complications.
Importance of Early Diagnosis and Treatment
Early diagnosis and treatment are crucial for improving the prognosis of acute pancreatitis. Prompt identification of the underlying cause and timely intervention can help prevent complications and reduce the risk of long-term damage to the pancreas.
- Early diagnosis:Prompt recognition of symptoms and seeking medical attention can allow for timely intervention and prevent complications.
- Treatment:Treatment focuses on managing pain, preventing complications, and supporting the body’s functions. This may include intravenous fluids, pain medications, and antibiotics.
Long-Term Outlook
Most patients with mild pancreatitis make a full recovery. However, severe cases can lead to long-term complications, such as chronic pancreatitis, pancreatic insufficiency, diabetes, and even death. The long-term outlook for individuals with pancreatitis varies depending on the severity of the disease, the presence of complications, and the patient’s adherence to treatment recommendations.
- Recovery:In mild cases, patients usually recover completely within a few weeks.
- Complications:Severe cases can lead to complications such as chronic pancreatitis, pancreatic insufficiency, diabetes, and even death.
Living with Acute Pancreatitis
Living with acute pancreatitis can be a challenging experience, but with the right knowledge and support, you can navigate this journey and improve your long-term health and well-being. Understanding the importance of lifestyle modifications, dietary changes, symptom management, and regular follow-up care is crucial in managing this condition effectively.
Lifestyle Modifications
Lifestyle changes are essential for managing acute pancreatitis and preventing future episodes.
- Avoiding alcohol and smoking:Alcohol and smoking are major risk factors for pancreatitis. Quitting these habits can significantly reduce your risk of future episodes and improve your overall health.
- Maintaining a healthy weight:Obesity is a risk factor for pancreatitis. Losing even a small amount of weight can help reduce your risk of developing the condition and improve your overall health.
- Managing stress:Stress can exacerbate pancreatitis symptoms. Finding healthy ways to manage stress, such as exercise, meditation, or yoga, can help improve your quality of life.
Dietary Changes and Nutritional Support
Dietary changes are crucial for managing acute pancreatitis.
- Specific dietary restrictions:Patients with pancreatitis often need to avoid fatty foods, alcohol, and caffeine. A registered dietitian can help create a personalized meal plan that meets your individual needs.
- Nutritional support:In some cases, patients may require nutritional support through intravenous feeding or enteral feeding tubes to ensure they are getting the nutrients they need.
- Role of a registered dietitian:A registered dietitian can provide guidance on dietary choices, help you understand the nutritional needs of pancreatitis, and offer counseling on managing your diet.
Managing Pain and Other Symptoms
Pain is a common symptom of acute pancreatitis.
- Common symptoms:Patients may experience severe abdominal pain, nausea, vomiting, fever, and jaundice.
- Pain management strategies:Pain management strategies include medication, pain relief techniques like heat therapy or massage, and complementary therapies like acupuncture or yoga.
- Managing other symptoms:Nausea and vomiting can be managed with anti-nausea medications, while fatigue can be addressed by getting enough rest and managing stress.
Regular Follow-Up with Healthcare Providers
Regular follow-up with healthcare providers is crucial for managing acute pancreatitis and preventing complications.
- Frequency of follow-up:The frequency of follow-up visits will depend on the severity of your condition and your individual needs. You may need to see your doctor every few weeks or months.
- Key aspects of follow-up care:Follow-up care includes monitoring for complications, assessing pain levels, reviewing medication needs, and discussing any changes in your condition.
- Early detection and management of potential complications:Early detection and management of potential complications, such as pancreatic pseudocyst or diabetes, are essential for improving your long-term health.
Living with Acute Pancreatitis: A Blog Post
A diagnosis of acute pancreatitis can be overwhelming, but it’s important to remember that you’re not alone. With the right knowledge and support, you can manage this condition and live a fulfilling life.
Here are some tips for living with acute pancreatitis:
- Make lifestyle changes:Quit smoking and alcohol, maintain a healthy weight, and find healthy ways to manage stress.
- Follow a healthy diet:Avoid fatty foods, alcohol, and caffeine. Work with a registered dietitian to create a personalized meal plan.
- Manage your symptoms:Talk to your doctor about pain management strategies, nausea relief, and ways to cope with fatigue.
- Attend regular follow-up appointments:This allows your doctor to monitor your condition, assess pain levels, and address any concerns.
- Connect with others:Joining a support group or online forum can provide valuable emotional support and connect you with others who understand what you’re going through.
Remember, living with acute pancreatitis is a journey, not a destination. With the right support and care, you can manage your condition and live a healthy and fulfilling life.
Research and Future Directions
Acute pancreatitis is a complex and often debilitating disease, and ongoing research efforts aim to improve our understanding of its causes, develop more effective treatments, and find ways to prevent it. Researchers are actively investigating various aspects of this disease, from its fundamental mechanisms to the development of novel therapies.
Current Research Areas
Current research endeavors focus on various aspects of acute pancreatitis, including:
- Pathogenesis and Mechanisms:Researchers are investigating the precise molecular and cellular events that trigger and contribute to pancreatitis. This includes studying the role of inflammatory mediators, digestive enzymes, and the immune system in the development of the disease.
- Genetic Predisposition:Studies are being conducted to identify genetic factors that may increase the risk of developing acute pancreatitis. This knowledge can help identify individuals at higher risk and potentially lead to personalized prevention strategies.
- Role of Microbiota:The gut microbiome is increasingly recognized as a key player in health and disease. Researchers are exploring the potential role of gut bacteria in the pathogenesis of acute pancreatitis and how manipulating the gut microbiome might influence disease severity.
- Novel Therapeutic Targets:Scientists are actively searching for new drug targets to treat acute pancreatitis. This includes investigating the role of specific enzymes, signaling pathways, and immune cells in the disease process.
- Improving Diagnostic Tools:Research is ongoing to develop more accurate and sensitive diagnostic tools for acute pancreatitis. This includes exploring the use of biomarkers, imaging techniques, and artificial intelligence algorithms.
Potential New Treatments and Therapies
The development of new treatments for acute pancreatitis is a major area of focus in research. Here are some promising areas of investigation:
- Anti-inflammatory Therapies:New drugs that target specific inflammatory pathways, such as those involving cytokines or chemokines, are being investigated to reduce inflammation and prevent organ damage.
- Enzyme Inhibitors:Research is underway to develop more effective inhibitors of digestive enzymes, such as trypsin and chymotrypsin, which are implicated in the damaging effects of pancreatitis.
- Stem Cell Therapy:Stem cells have shown potential in regenerating damaged pancreatic tissue. Clinical trials are exploring the use of stem cells to promote healing and restore pancreatic function.
- Gene Therapy:Gene therapy approaches aim to modify gene expression to prevent or treat pancreatitis. This includes delivering genes that encode protective proteins or inhibit harmful enzymes.
- Immunotherapy:Immunotherapy strategies are being investigated to modulate the immune response in pancreatitis, reducing inflammation and promoting healing.
Understanding the Pathogenesis of Pancreatitis
A deep understanding of the pathogenesis of pancreatitis is crucial for developing effective therapies and preventive measures. Researchers are using a variety of techniques to unravel the complex mechanisms involved in this disease. These include:
- Animal Models:Animal models, such as mice and rats, are used to study the disease process in a controlled setting. This allows researchers to manipulate variables and investigate the effects of different treatments.
- Cell Culture Studies:In vitro studies using pancreatic cells grown in the laboratory allow researchers to examine specific cellular and molecular events involved in pancreatitis.
- Biomarker Analysis:Researchers are identifying and analyzing biomarkers in blood and other bodily fluids to monitor disease progression and assess the effectiveness of treatments.
- Imaging Techniques:Advanced imaging techniques, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), are being used to visualize the pancreas and assess the extent of inflammation and damage.
Search for Effective Preventive Strategies
Preventing acute pancreatitis is a key goal of research. Current efforts focus on:
- Lifestyle Modifications:Studies are investigating the impact of lifestyle factors, such as alcohol consumption, smoking, and diet, on the risk of developing pancreatitis. This information can be used to develop public health recommendations for reducing risk.
- Early Detection and Intervention:Researchers are exploring ways to identify individuals at high risk for pancreatitis early on. This includes developing screening tools and implementing preventive measures in high-risk groups.
- Targeting Risk Factors:Research is underway to develop therapies that target specific risk factors for pancreatitis, such as gallstones or alcohol abuse.
Types of Acute Pancreatitis
Acute pancreatitis is a serious condition that occurs when the pancreas becomes inflamed. The pancreas is a gland that produces enzymes that help digest food and hormones that regulate blood sugar. When the pancreas becomes inflamed, these enzymes can start to digest the pancreas itself, causing damage.
There are several different types of acute pancreatitis, each with its own cause, symptoms, and treatment. Understanding these different types is important for effective diagnosis and management.
Types of Acute Pancreatitis
| Type | Cause | Symptoms | Treatment |
|---|---|---|---|
| Alcoholic Pancreatitis | Excessive alcohol consumption | Severe abdominal pain, nausea, vomiting, fever, and jaundice | Abstinence from alcohol, pain management, intravenous fluids, and nutritional support |
| Biliary Pancreatitis | Gallstones blocking the common bile duct | Similar to alcoholic pancreatitis, but may also include symptoms of biliary obstruction, such as jaundice and dark urine | Pain management, intravenous fluids, and endoscopic retrograde cholangiopancreatography (ERCP) to remove the gallstones |
| Idiopathic Pancreatitis | Unknown cause | Similar to alcoholic and biliary pancreatitis | Pain management, intravenous fluids, and nutritional support |
Complications of Acute Pancreatitis
Acute pancreatitis can lead to a range of complications, some of which can be life-threatening. These complications can arise from the inflammatory process itself or from the body’s response to the inflammation. Early diagnosis and treatment of acute pancreatitis are crucial to prevent complications and improve patient outcomes.
Complications of Acute Pancreatitis
| Complication | Description | Symptoms | Treatment |
|---|---|---|---|
| Pancreatic Necrosis | Death of pancreatic tissue due to severe inflammation and lack of blood supply. | Severe abdominal pain, fever, elevated heart rate, and signs of infection. | Antibiotics, surgical debridement, and supportive care. |
| Infection | Bacterial infection of the pancreas or surrounding tissues. | Fever, chills, increased pain, and signs of sepsis. | Antibiotics and drainage of infected fluid. |
| Fluid Accumulation | Build-up of fluid in the abdomen (ascites) or around the pancreas (pancreatic pseudocyst). | Abdominal distension, shortness of breath, and weight gain. | Drainage of fluid, medications to reduce fluid accumulation, and supportive care. |
| Organ Failure | Failure of vital organs, such as the lungs, kidneys, or heart, due to the inflammatory response or complications of pancreatitis. | Shortness of breath, decreased urine output, and signs of heart failure. | Supportive care, including mechanical ventilation, dialysis, and medications to support organ function. |
| Bleeding | Bleeding within the pancreas or surrounding tissues. | Severe abdominal pain, hematemesis, and melena. | Blood transfusions, surgery to control bleeding, and medications to stop bleeding. |
Early diagnosis and treatment of acute pancreatitis are essential to prevent complications. Prompt medical attention can help reduce the risk of severe complications, such as pancreatic necrosis, infection, and organ failure. If you experience symptoms of acute pancreatitis, such as severe abdominal pain, fever, and nausea, seek immediate medical care.
Illustration: Pancreas Anatomy
The pancreas is a vital organ that plays a crucial role in digestion and blood sugar regulation. Understanding its anatomy is essential for comprehending how pancreatitis develops and how it affects the body.
Pancreas Anatomy
The pancreas is a long, flat organ located in the upper abdomen, behind the stomach. It is connected to the small intestine via the pancreatic duct. The pancreas has three main parts: the head, body, and tail.
- Head:The widest part of the pancreas, located in the curve of the duodenum (the first part of the small intestine).
- Body:The middle section of the pancreas, which lies behind the stomach.
- Tail:The narrowest part of the pancreas, extending towards the spleen.
The pancreas contains two types of tissue: exocrine and endocrine.
- Exocrine tissuemakes up the majority of the pancreas and produces digestive enzymes that are released into the small intestine through the pancreatic duct. These enzymes help break down carbohydrates, fats, and proteins into smaller molecules that can be absorbed by the body.
- Endocrine tissueis made up of clusters of cells called islets of Langerhans, which produce hormones that regulate blood sugar levels. The most important hormones produced by the islets are insulin and glucagon.
Role of the Pancreas in Digestion and Hormone Production
The pancreas plays a crucial role in digestion by producing digestive enzymes that break down food. These enzymes are released into the small intestine through the pancreatic duct.
- Amylasebreaks down carbohydrates into simple sugars.
- Lipasebreaks down fats into fatty acids and glycerol.
- Proteasesbreak down proteins into amino acids.
The pancreas also produces hormones that regulate blood sugar levels. Insulin lowers blood sugar levels by promoting the uptake of glucose from the bloodstream into cells. Glucagon raises blood sugar levels by stimulating the liver to release stored glucose into the bloodstream.
Pancreas Diagram
[Describe the diagram here, including labels for the head, body, tail, pancreatic duct, islets of Langerhans, and surrounding organs.]
Importance of the Pancreas
The pancreas is a vital organ that plays a crucial role in digestion and blood sugar regulation. Its functions are essential for maintaining overall health. Without a properly functioning pancreas, the body would be unable to properly digest food or regulate blood sugar levels, leading to a range of health problems.
Illustration: A Student Learns What Information About Acute Pancreatitis
Acute pancreatitis is a serious condition that can lead to significant complications. To understand this condition better, let’s delve into the inflammatory process involved.
Inflammation and Tissue Damage
Acute pancreatitis is characterized by inflammation of the pancreas, a gland located in the upper abdomen. This inflammation is triggered by the activation of digestive enzymes within the pancreas itself. Normally, these enzymes are inactive and stored within the pancreas.
However, in acute pancreatitis, these enzymes become prematurely activated, causing damage to the pancreatic tissue.
Pancreas Anatomy During Acute Pancreatitis
The pancreas is a long, thin organ that sits behind the stomach. During acute pancreatitis, the pancreas becomes inflamed and swollen. Areas of necrosis, or tissue death, can develop, especially in the areas where the enzymes are activated. The inflammation and necrosis can extend beyond the pancreas, affecting surrounding organs.
Complications
The inflammation and tissue damage in acute pancreatitis can lead to several complications, including:
- Fluid Accumulation:The inflammation can cause fluid to accumulate in the abdomen, leading to a condition known as ascites. This fluid can compress the organs, making it difficult for them to function properly.
- Organ Failure:The inflammation can also damage other organs, such as the lungs, kidneys, and heart. This can lead to organ failure, which can be life-threatening.
ERCP Procedure
ERCP, or endoscopic retrograde cholangiopancreatography, is a minimally invasive procedure that allows doctors to visualize and treat problems in the bile ducts and pancreas. This procedure is particularly helpful in diagnosing and treating pancreatitis.
ERCP Procedure Description
ERCP involves inserting a thin, flexible endoscope through the mouth, down the esophagus, into the stomach, and finally into the duodenum, the first part of the small intestine. The endoscope is equipped with a camera and various tools, including a biopsy forceps, an injection needle, and a balloon catheter.
The procedure typically begins with the patient being given sedation to ensure comfort. The endoscope is then carefully inserted into the digestive tract, guided by the camera’s live feed. Once the endoscope reaches the duodenum, a small, flexible tube called a cannula is inserted into the opening of the bile duct.
Contrast dye is then injected through the cannula, allowing the bile ducts and pancreas to be visualized on an X-ray screen. This visualization allows doctors to identify the cause of pancreatitis, such as gallstones, tumors, or other abnormalities. The endoscope’s tools can also be used to remove gallstones, dilate narrow bile ducts, or place stents to relieve blockage.
ERCP Use in Pancreatitis Diagnosis and Treatment
ERCP plays a crucial role in both diagnosing and treating pancreatitis. Here are some specific examples:
- Diagnosis:ERCP can help determine the underlying cause of pancreatitis, such as gallstones in the common bile duct, a tumor in the pancreas or bile duct, or a stricture (narrowing) in the bile duct. This information is essential for tailoring the appropriate treatment plan.
- Treatment:ERCP can be used to remove gallstones that are blocking the bile duct, a common cause of pancreatitis. The procedure can also be used to dilate narrowed bile ducts, allowing bile to flow freely and preventing further damage to the pancreas.
Additionally, ERCP can be used to place stents in the bile duct, which can help relieve blockage and prevent further pancreatitis episodes.
ERCP Risks and Complications
While ERCP is generally a safe procedure, potential risks and complications do exist. These include:
- Bleeding:Bleeding from the bile duct or pancreas can occur during the procedure.
- Pancreatitis:ERCP itself can sometimes trigger pancreatitis.
- Infection:Infection can occur after the procedure, though this is uncommon.
- Perforation:A hole can be made in the bile duct or pancreas during the procedure, which can lead to serious complications.
Patient Education and Informed Consent
Patient education and informed consent are crucial before undergoing any medical procedure, including ERCP. Patients should be fully informed about the benefits, risks, and alternatives to the procedure. This ensures that they can make an informed decision about their care.
Comparison of ERCP with Other Options
| Feature | ERCP | Other Options |
|---|---|---|
| Diagnostic Accuracy | High | May vary depending on the option |
| Treatment Effectiveness | High for specific conditions | May vary depending on the option |
| Risks and Complications | Potential for bleeding, pancreatitis, infection, perforation | May vary depending on the option |
| Cost | Generally higher | May vary depending on the option |
ERCP Resources
Patients considering ERCP may find the following resources helpful:
- Websites:The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), The American Gastroenterological Association (AGA)
- Patient Support Groups:The Pancreatitis Foundation, The Crohn’s & Colitis Foundation
- Medical Professionals:Gastroenterologists, Hepatologists
Popular Questions
What are the most common causes of acute pancreatitis?
The most common causes of acute pancreatitis include gallstones, alcohol abuse, and certain medications.
Is acute pancreatitis contagious?
No, acute pancreatitis is not contagious. It is caused by inflammation of the pancreas, not by a virus or bacteria.
What is the long-term outlook for people with acute pancreatitis?
The long-term outlook for people with acute pancreatitis depends on the severity of the condition and the presence of complications. With proper management, most people recover fully, but some may develop chronic pancreatitis or other long-term health problems.
What are some things I can do to prevent acute pancreatitis?
You can reduce your risk of acute pancreatitis by avoiding alcohol abuse, managing gallstones, maintaining a healthy weight, and eating a balanced diet.